- What Do 2 Brown Lines on the Nail Mean?
- Muehrcke’s lines
- COVID-19
- Phylloderma
- Cyanosis
- Splinter hemorrhage
- Psoriasis
- Skin Cancer, Fee Splitting, RAC Audits, Physician Extenders, and the Role of the Government in Healthcare Fraud
- Skin cancer
- Fee splitting
- RAC audits
- Physician extenders
- ‘Level of care’ documentation
- Pinnacle dermatology
What Do 2 Brown Lines on the Nail Mean?

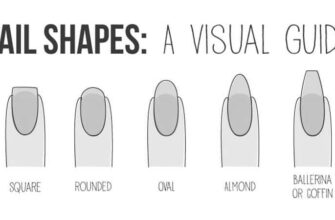
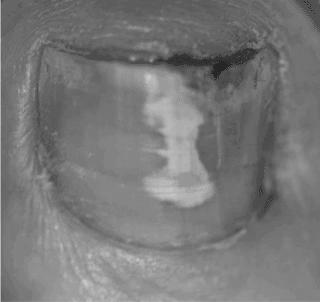
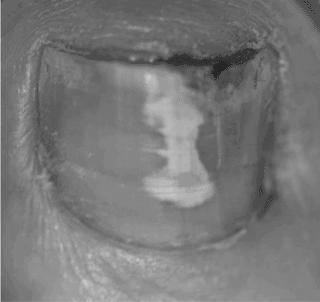
What do two brown lines on the nail mean? These stripes are caused by a condition known as linear melanonychia. This condition is considered a normal variation of fingernail color and results when the pigments in the nail produce too much pigment. This causes the pin to appear darker than it is. Linear melanonychia affects nearly 50% of African-Americans. Linear melanonychia may also be caused by a condition called splinter hemorrhage.
Muehrcke’s lines

Unlike many other diseases, Muehrcke’s lines are not caused by physical trauma to the nail. Instead, they result from low protein levels found in the blood called albumin. Albumin helps carry nutrients throughout the body, so when the blood levels fall below 2.2 g/dL, the white bands will appear on the nail. In addition to chronic hypoalbuminemia, other causes include chemotherapy drugs, high altitude, and other metabolic conditions.
Symptoms of Muehrcke’s lines are similar to those of Beau’s lines on the nail. The difference is that Muehrcke’s lines occur on more than one nail. The condition is usually reversible. Mees’ lines will disappear when the protein levels return to normal. They typically do not grow with the nail. They may disappear on their own.
Fortunately, Muehrcke’s lines on the nail are treatable. Despite their appearance, they are primarily cosmetic and often improve with treatment of an underlying illness. In addition to addressing the underlying problem, Muehrcke’s lines signify a condition that needs to be treated. The most common treatment options include medication and surgery. But if the situation is not treatable, Muehrcke’s lines may signify something more serious.
It can result in seizures and coma. Another cause is a highly contagious virus known as mumps. The symptoms of mumps may also affect the reproductive system. Additionally, if not appropriately treated, it can cause damage to the heart, pancreas, and brain.
COVID-19

This virus may cause two brown lines on the nail. These are known as Beau’s lines. This condition affects people with viral illnesses and is often caused by the stress of fighting off the virus. If COVID-19 is detected early, the lines may be curable or grow out. If you see these lines on your nail, you should consult a doctor as soon as possible.
If you’re concerned about a COVID-19 infection, these lines may indicate this condition. They appear two to three weeks after you’re diagnosed. They appear above the lunula, a white part near the base of the nail. Symptoms typically go away in a few days, but it’s always best to visit a doctor if you have a red half-moon on your nail. If you’re embarrassed to show people your nails, consider using a mask or distancing yourself socially. If your pin has a red half-moon, don’t share your identity with anyone! You may be contagious!
Other nail changes may be caused by COVID-19. They include orange-brown nail discoloration and a tinge of luminescence under Wood’s light. However, if these changes persist or worsen after recovering from the illness, they are not COVID-19-related. In addition, nails may be affected by various diseases and medications that cause nail changes.
Phylloderma

Two brown lines under the fingernail are not a sign of cancer. They are simply the result of an abnormality in the nail’s pigments. Symptoms of this disorder usually start with recent changes in the lines. If the lines have become darker in color, it may be a complication of a vascular condition, such as acute renal failure, heart failure, ulcerative colitis, or breast cancer. Brown-black lines under the nail may result from trauma or bacterial or fungal infection. Exogenous pigmentation may also be a factor, as excess melanin is produced in the nail matrix.
Cyanosis
If you’re wondering if two brown lines on the nail mean cyanoses, you’re not alone. There are several other common symptoms of cyanosis, including difficulty breathing and confusion. You may also have chest pain, a high fever, or a cough with dark mucus. Your doctor will perform a physical exam, focusing on your heart and lungs. They’ll also likely use a pulse oximeter to monitor your oxygen saturation.
First of all, what exactly is cyanosis? Cyanosis is a condition that occurs when the blood isn’t carrying enough oxygen to the tissues. Maybe most noticeable on the nailbed and lips. Cyanosis is derived from the Greek word, which means dark blue. It’s often an underlying problem that needs immediate medical attention.
There are several different causes of cyanosis. When red blood cells aren’t carrying enough oxygen to the rest of the body, they turn blue. The condition can be caused by many factors, including poor circulation and lung problems. It can also result from trauma or a zinc deficiency. You may also have a low zinc level, which can lead to blue fingernails.
Cyanosis is caused by a bacterium called Pseudomonas in the blood. This bacterium can be found in damp environments, but if a different condition causes it, the infection is likely to be cured. Treatment for this condition is challenging and often requires the collaboration of several specialists. However, it is essential to remember that a weakened blood supply usually causes cyanosis in the skin and nails.
Splinter hemorrhage

It can take several months for the blemish to disappear in some cases. However, it can also be a sign of a more severe condition. Your nail technician should monitor the area for widening and spreading hemorrhage signs. If it appears to apply, it may be a melanoma.
There are a few different causes of splinter hemorrhages. Some of these are trauma to the nail, such as stubbing. Typically, this does not require treatment and will disappear within a few days. A fungal infection can also cause a black line on the nail. A fungal infection is the most likely cause of the line. Fungal infections are the most common cause of nail hemorrhages.
Unlike splinter hemorrhage, two brown lines on the nail mean spike hemorrhage. The nail can look like a splinter because the blood discoloration runs in the direction of growth. Often, the blood color is reddish-brown, similar to the color of a wooden fragment. However, it is best to consult your doctor if it persists for more than two days.
Psoriasis

If you’re wondering, “Do two brown lines on the mean nail p.soriasis?” you aren’t alone. Many people suffer from this condition, and there are some simple things you can do to prevent it. First, make sure you’re not allergic to nail polish, which can exacerbate the condition. Next, don’t pick at the nail, as it could loosen and infect the skin beneath. Instead, soak the affected nail in warm water to remove debris and prevent infections.
The gradual separation of the nail from the skin is painless, but it can create a pathway for infection. About one-third of people with nail psoriasis develop a fungal infection. This type of infection is often painful, and the buildup of dead skin cells under the nail can be pretty uncomfortable. To make sure that the pin isn’t infected.
If the discoloration is severe, a doctor should examine the nails thoroughly to rule out a more severe condition. The nail may be lifting from the finger and forming an oil spot. If the pin is crumbling, splinters may have formed beneath it. This condition is treatable, but it is still essential to see a physician for a proper diagnosis. You probably have psoriasis if you notice two brown lines on your nail.
Skin Cancer, Fee Splitting, RAC Audits, Physician Extenders, and the Role of the Government in Healthcare Fraud

In this article, we’ll discuss skin cancer, fee-splitting, RAC audits, Physician extenders, and the role of the government in healthcare fraud. You may be wondering how to protect yourself and your practice from a potential rap. Here are three ways to keep your routine from becoming a scam:
Skin cancer

The rise in the prevalence of melanoma has resulted in more than 200,000 new cases and 55,000 deaths globally in 2012. According to the World Health Organization, there were 13,134 new cases in Australia in 2014 and 23,414 points in New Zealand in 2010. In the USA, it is expected that there will be 75,870 new cases and 9940 deaths in 2014. The highest incidence was reported in Scandinavian countries, north-western Europe, and Switzerland.
It is important to remember that advanced techniques for detecting skin cancer may increase false-positive diagnoses and increase the risk of misdiagnoses. Furthermore, dermoscopy is not a substitute for a thorough history-taking and clinical examination of the entire body. Again, many branches of medicine have noted the danger of gizmo idolatry. Dr. Coldiron is skeptical of the widespread use of dermoscopy in primary care and recommends that clinicians use a thorough physical examination and clinical history-taking to ensure a proper diagnosis.
There are several methods of determining whether a mole is cancerous. A visual skin check can detect any suspicious moles or other skin abnormalities. However, it cannot make a definitive diagnosis. A biopsy is needed to determine the presence of cancer. A physician will numb the area on which a mole is located before removing it. The sample is then sent to a lab, where a pathologist will check for cancer cells.
Fee splitting

Some red flags indicate that fee-splitting in dermatology is a scam. First, you need to hire the right legal and business advisers. It would help if you understood the difference between group and individual valuation based on free cash flow. Physicians valued their practices based on accounts receivable, equipment, and a goodwill factor in the past. If you are considering fee-splitting, you should consider all of these factors before deciding.
Another red flag is when a pathologist charges for slide work that a dermatologist did not perform. Pathologists frequently assess patients for work completed elsewhere, but dermatologists mark it on the patient’s bill. Many pathologists consider this practice unethical and argue that dermatologists simply corner the market. While it’s true that a dermatologist may not be the one doing the work, the patient benefits from dealing with a single party.
If you’re unsure whether or not fee-splitting is an ethical practice, contact the MFCU. The MFCU recently enforced a new law prohibiting fee-splitting, preventing many physicians from engaging in this practice. A bill was introduced in the New York State Senate in 2015 that would have allowed hospitals to pay practice management vendors based on a percentage of the fees they charge doctors. However, physicians should continue scrutinizing any proposed arrangement.
RAC audits

If you are a dermatologist, you have probably heard about RAC audits of dermatology practices. While they are not a scam, they can be intimidating. These audits are designed to prevent fraud and may also be referred to the Department of Health and Human Services Office of Inspector General Office of Investigations. These audits are conducted by recovery audit contractors (RACs), who are hired by the government and are paid on a contingency basis. Recovery audit contractors are investigating healthcare practices in different geographic regions. They are looking for under-documented services, inaccurately coded and billed services, and overpayments.
Practices must ensure compliance with all regulations and policies. It will help eliminate any occurrences of fraud and protect revenue and practice reputation. Moreover, documentation of a patient should not be copied from a previous visit. Copy-pasting can result in confusing information, incorrect coding, and potential fraud. Additionally, mistakes in documentation violate HIPPA rules and expose the physician to potential fraud.
The RAC auditors also require health care providers to follow complex audit procedures. Using medical records, they determine whether a specific claim is incorrect or whether a service was medically necessary. In addition to the RAC audit process, contractors are paid based on the number of shares they can collect. While most RAC auditors do not have medical backgrounds, they require a bachelor’s degree. Furthermore, RAC audit contractors are paid on a contingency basis, and their incentive is to collect as much as possible. As such, they are more likely to be aggressive with their audits.
Physician extenders

Dermatology practices are utilizing physician extenders to cut wait times. Physician extenders are not board-certified physicians in dermatology, including physician assistants and nurse practitioners. The evolution of the dermatology workforce raises questions about the future of practice models and patient outcomes. A recent study found that patients in Ohio wait 56 days to see a dermatologist. But should dermatology practices use physician extenders?
A physician extender can bill for services even when the physician isn’t physically present in the office. However, new Medicare rules clarify this rule. Therefore, it’s best to avoid dermatologists who bill you for services you didn’t receive. When you’re considering whether to see a dermatologist, check his Medicare data. Make sure to ask if he bills independently or is a physician extender.
The Modernizing Medicine site provides sample forms and templates for physicians. However, it is essential to understand that the Modernizing Medicine site is not a health care provider. The referenced forms and templates are provided for educational purposes only. These documents should be finalized by the physician who provides the care. Nonetheless, these services are not worth the cost. Instead, you’ll be wasting your time. The only way to ensure patient safety and satisfaction is to find a physician you trust.
‘Level of care’ documentation

One example of ‘Level of care’ documentation in dermatologic scams involves the doctor charging Medicare for unnecessary procedures performed by unqualified physician assistants. In a case where the doctor set Medicare for $49 million worth of unnecessary procedures, the physician was allegedly overseas while performing some of the systems—which led to false billing and Medicare payments totaling $49 million over six years. A similar example involves a physician who misdiagnoses a patient’s condition and charges Medicare for unnecessary medical services.
‘Level of care’ documentation in dermatologic scams can be spotted when the doctor bills for services they did not perform. The doctor may also bill for services rendered when the patient was not present in the office or out of the country. In another instance, the physician may work for an impossible number of hours, such as 26 hours in a single day. It may be a fraud to claim a “high level of care” when there is no such documentation.
- Derm’s office
What percentage of dermatology as practiced is fraudulent? According to a recent survey, the answer may surprise you. Some dermatologists delegate payment collection to the nursing staff at a medical center. Others collect payment before performing specific techniques. If you were to ask the average dermatologist how much she bills per patient, she would say that she charges a flat $45 fee. In addition, a third of dermatologists admit to charging patients in violation of Medicare guidelines.
Private equity-backed dermatology practices often try to increase revenue by acquiring their labs. This additional revenue can pay for extra tests that the dermatologist may not perform. This scenario is prevalent with practices owned by private equity firms. In a recent study published in the American Academy of Dermatology Journal, Pinnacle Dermatology, a Tennessee-based dermatology group, employed more nurse practitioners than physicians. The study uncovered the negative impact of private equity-owned dermatology practices.
Private equity-backed dermatology practices have become the focus of takeovers and mergers. The highly fragmented market does dermatology practices an attractive investment for private equity funds. As a result, researchers identified more than 30 dermatology practice acquisitions in the United States. While these acquisitions are often beneficial for patients, they can also lead to problems for the practice owner. Increasing demand from private equity buyers means less competition for doctors and more profit for practice owners.
Pinnacle dermatology
Private equity firms have been implicated in several adverse outcomes in dermatology and have been linked to a greater reliance on physician extenders, such as nurse practitioners, rather than physicians. According to Rios, nearly 15 percent of dermatology practices are owned by private equity.
The Pinnacle dermatology office, which Brown attended, failed to follow the American Board of Dermatology standards. Pinnacle’s laboratory is certified by the College of American Pathologists and is subject to federal regulations under the Clinical Laboratory Improvement Amendments. Pinnacle’s owner, Dr. Sailesh Konda, is an associate clinical professor of dermatology at the University of Florida. He has conducted extensive research into how private equity companies affect the field of dermatology.
This study examined patient-generated reviews on two consumer review websites: Yelp and ZocDoc. These consumer-focused platforms let patients rate dermatology practices on their overall satisfaction. Patients from 3 different cities were included in the analysis in this study. A high rating for the quality of care, efficiency, and practice competence was associated with positive reviews. The study also examined whether physicians’ demeanor and the quality of medical processes were related to patient satisfaction.