Will a Fingernail Grow Back After Acute Paronychia?
There are several treatments for acute and chronic paronychia. These treatments include antibiotics, antifungal tablets, and surgery. Regardless of your treatment, frequent hand-wetting should be addressed to improve your nails. You should wear gloves while working and handling your hands to avoid the risk of infection. If you have the condition, you should also avoid biting your nails, pushing back the cuticles, and manicuring the folds in your pin. You should also refrain from using nail varnish until the problem is cured.
Treatment of chronic paronychia

Chronic paronychia can be caused by several things, including trauma to the nail fold or cuticle. Sometimes, this trauma is minor and is caused by handwashing, finger sucking, or nail trimming. However, the problem is more severe in some cases and requires more invasive treatment. To determine the best course of treatment for chronic paronychia, your doctor will most likely recommend antibiotics.
The treatment for chronic paronychia usually involves modifying the causes of the problem. You should avoid touching your fingers with wet materials, such as water, and use a pair of cotton-lined waterproof gloves. Wash your hands with antibacterial soap and follow it up with hand cream. You may also be prescribed antibiotics. The doctor may drain the affected area to clear it in severe cases. If treatment is unsuccessful, you may need to repeat the process.
A comprehensive examination will help diagnose the cause of your paronychia. A physician will also check for any malignancy. After trying several medical treatments, you may need surgery if the condition persists. The goal of surgery is to remove the inflamed tissue, which will help the medication penetrate into the affected area and regenerate the cuticle. If you’ve already tried everything else and still can’t get rid of the paronychia, you may want to consult a dermatologist to get more information.
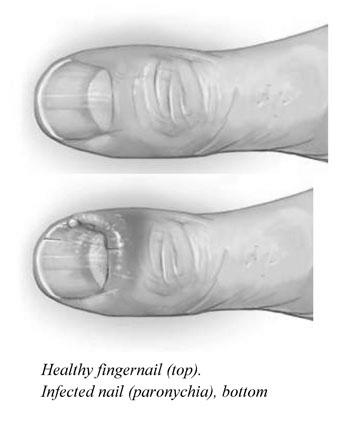
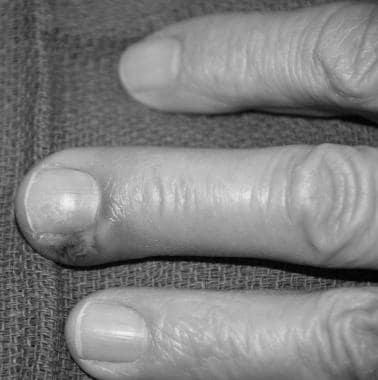
Patients who have had frequent contact with water should undergo an examination. The infection usually results in thickened nail folds, which is the hallmark of chronic paronychia. Depending on the severity of the condition, it may even be associated with felonies. It can be more severe if you have diabetes, a lower immune system, or a compromised immune system. Chronic paronychia may also be caused by Herpes simplex or Candida albicans.
The best way to treat chronic paronychia is to identify its cause and treat it. There are many causes of the condition, including regular hand wetting and immune system conditions. Although the role of Candida is still unknown, chronic paronychia is often the result of irritant dermatitis with secondary fungal colonization. You should consider the following treatments for chronic paronychia.
Candida is the most common cause of paronychia. This yeast-like organism causes periungual erythema and edema. Treatment for chronic paronychia requires a combination of prescription antibiotics, over-the-counter medications, and home remedies. If the symptoms of chronic paronychia persist or are established, you should consult your doctor. They will prescribe you an appropriate prescription.
Acute paronychia occurs when a nail fold becomes inflamed. Treatment involves drainage of the purulent fluid, soaks, and topical antibacterials. However, chronic paronychia develops as the protective tissues of the nail fold are damaged. If left untreated, it can lead to an abscess and even infection. As a result, the best treatment for chronic paronychia is to avoid water altogether.
If you have a severe case of paronychia or are diabetic, you should see a doctor immediately. A doctor can diagnose by inspecting the area and testing a sample of pus for bacteria or fungi. The length of time that paronychia lasts will depend on the type and the cause. Treatment may also involve surgical drainage of the affected nail fold.
Treatment of acute paronychia

Acute paronychia can be treated with warm water soaks and an antiseptic solution. Treatment for bacterial causes involves topical antibiotics. Early drainage of an abscess prevents the infection from spreading to the hand’s tendons. If chronic paronychia is the cause, the condition can be treated with steroid cream. Antibiotics should be taken for a few weeks to see complete improvement.
While the clinician may diagnose the infection and prescribe a course of treatment, the pharmacist may be able to recommend antimicrobial therapy and detect any drug interactions. Nursing staff can monitor patient compliance, counsel patients about the medication, and report issues to the prescribing clinician.
The treatment for acute paronychia depends on the cause and severity. Whether or not pus is present in the nail folds is essential for diagnosis. If pus is present, the doctor may recommend a systemic antibiotic to fight off the infection. Flucloxacillin or Clindamycin, taken four times daily, can be prescribed. If these antibiotics fail, the patient may need systemic treatment.
Diagnosis is crucial, as the rash can progress to osteomyelitis if left untreated. Diagnosis is often complicated by a complication. In severe cases, recurrent infections can be caused by herpes simplex, fungus, or a combination of the two. In some cases, the condition can be mistaken for another state and require a biopsy. A diagnosis of acute paronychia requires treatment.
Depending on the severity of the infection, treatments may reduce the pain and swelling of the infected toe. In many cases, soaking the affected foot or hand in a warm antiseptic solution every day for about 20 minutes can relieve the symptoms. In more severe cases, a doctor may sample the pus and prescribe an antibiotic or antifungal topical to help reduce the infection.
Acute paronychia is usually self-limited, lasting about five to ten days. The condition is generally harmless and does not lead to permanent damage to the nail, but the disease may progress to osteomyelitis in very severe cases. Chronic paronychia may require antifungal medication for weeks. Acute paronychia can recur due to injuries or improper care of the affected nail area.
The treatment of chronic paronychia includes avoiding contact irritants and using a broad-spectrum antifungal agent or corticosteroid. In addition to drug treatments, topical steroid creams may help. If drug treatments are ineffective, en bloc excision of the proximal nail fold may be an option. A proximal marsupialization of the nail fold may also be effective.
Acute paronychia is a painful infection of the nail folds. The affected area will be red and swollen and may contain pus or a small blood collection. In some severe cases, the condition may penetrate the nail plate deep into the finger or toe. This type of infection occurs mainly in individuals with poor circulation. Acute paronychia is a painful condition. If left untreated, it could lead to a severe hand infection.
Acute paronychia results from bacterial infection of the nail folds. In acute paronychia, the nail fold is inflamed, and a purulent fluid will form around it. Sometimes pus may include, but that is rare. Chronic paronychia is caused by bacterial infection and involves frequent exposure to water. The causative organism is a fungus called Candida. It is best to avoid the water until the condition is under control.
The infection may be self-limiting in acute paronychia and does not require antibiotics. If an abscess is present, surgical intervention may be needed.
In addition to over-the-counter medications, medical treatment for acute paronychia can involve surgical intervention. A small hemostat or #11 scalpel blade can drain fluid in some cases. A thin gauze wick may be placed under the impacted nail. If the inflammation is severe enough, a small needle inserted into the area will be able to remove it. A physician can perform a biopsy to determine the source of the infection.
What Causes Orange Fingernails?

What causes someone to have orange fingernail color? Some health issues or vitamin deficiencies are the cause of orange fingernails. Vitamin deficiencies are treatable by a doctor, but sometimes more severe conditions cause orange nails. A simple home remedy for orange fingernails can help you remove the color. One home remedy involves lemon and baking soda solution. Another method uses tea tree oil. To apply the tea tree oil, you need to mix the two ingredients together and then dab the nail. You should allow it to sit for about 3 minutes before wiping it off with clean water.
Symptoms

Some people experience discoloration of their fingernails due to an unhealthy diet, vitamin deficiencies, and overexposure to orange and red-colored nail polish. However, in some cases, discoloration of fingernails may be an indicator of more severe health conditions, such as a lack of hemoglobin or a liver problem. In addition, orange fingernails may be indicative of diabetes.
Fungal infections or other health conditions can also cause orange nails. If you’re worried about this, you should consult a doctor immediately. The orange nail stain can be removed with over-the-counter medication or a home remedy in some cases. Applying a solution of lemon juice and baking soda to your fingernails can remove the discoloration within a few minutes. Another method involves applying tea tree oil to your fingernails. This method requires the use of a clean toothbrush and nail brush. Be patient and follow the instructions to prevent further discoloration.
Several causes of orange fingernails can be caused by a bacterial infection of the nail fold. This infection affects the skin surrounding the nail and causes redness, inflammation, and pus. In severe cases, the nail may be thickened and discolored. Some people also experience white fingernails due to trauma. While these conditions are not extreme, proper medical attention is needed to treat the problem. A simple visit to your doctor will help you determine if this is the case.
Causes

There are several causes of orange fingernails, including vitamin deficiency, eating too many carrots and sweet potatoes, and various environmental factors. Sometimes the discoloration is a sign of an underlying condition, such as a fatty liver, lack of hemoglobin, or even diabetes. Although the underlying cause is unknown, you should consult a physician if the discoloration is severe.
The condition of your nails is an essential indicator of your health, and any color changes can be alarming. If you notice your nails turning orange, you should immediately visit a physician to determine whether they signify a health problem or incorrect use of nail care products. If the change results from stress or anxiety, relaxation techniques can be helpful. In addition, it can be the result of an untreated nail polish stain.
Other causes of orange fingernails include a fungal infection of the nail beds or too much beta carotene consumption. However, if you suspect a fungus, you should consult your doctor or pharmacist. You can try a home remedy for orange fingernails as well. To remove the stain, soak your fingers in diluted hydrogen peroxide. The process may take a while, but a clean toothbrush can help.
Treatments

What causes orange fingernails? Many factors, including nail polish and fungal infection, can cause orange fingernails. Fungal infections are caused by a fungus known as onychomycosis. The condition causes the nails to thicken and separate from the nail beds. If you have orange toenails, you might want to get tested for diabetes to find out why you have them.
An easy way to treat your discolored nails is by using tea tree oil. You can apply this oil directly to your fingernails and then mix it with a carrier oil like olive, coconut, or jojoba oil. Tea tree oil is another excellent option, as it can prevent fungus growth. Since it’s alkaline, tea tree oil prevents fungus from spreading. The oil can also make your nails look better.
Oral antifungals can be helpful, but they are not a permanent cure. Antifungal medications have a low cure rate. A single course of antifungal medicines may only cure a portion of the infection, so you may need to repeat it. In some cases, a dermatologist can culture your nails and prescribe a treatment specifically targeted at the fungus. By following these steps, you can get rid of your orange fingernails.
Another natural solution for orange fingernails is to soak your nails in lemon juice. The lemon juice will help remove nail polish. It can also help remove yellow nail staining. Applying lemon juice on your nails will also bring out natural white tips. If you cannot afford to visit a salon, there are many ways to fix your problem at home. You can also try baking soda on your nails. You should repeat this treatment every six to eight weeks.
Ingrown toenail

A common foot problem is an ingrown toenail. Ingrown toenails can be caused by various factors, including over-polishing, improper nail clipping, or fungal infection of the nail. An ingrown toenail does not pose a health risk for most people, but it can result in painful, red, swollen, or even orange fingernails if it is left untreated.
While you may have a tan, a yellow or orange toenail may indicate a different condition. If your toenail is green and a greasy, warty, or foul-smelling substance appears underneath, it may signify Darier’s disease. Fortunately, this inherited condition is easy to detect and treat if you tend to ingrown toenail symptoms.
While a home remedy can relieve some of the pain, it is not a long-term solution. If the pain persists or the ingrown toenail recurs, you should see a doctor. Home treatments may only relieve the pain for a day or two, but if you cannot walk or perform any strenuous activity, you should consult a medical professional. Depending on the severity of the condition, you may need surgery.
The best home treatment for an ingrown toenail is soaking the foot in warm water for at least 20 minutes. You can also apply a topical antibiotic to the affected area. If the infection is not present, it may be cured with a visit to a podiatrist. In addition, people with diabetes, poor circulation, or nerve damage may be particularly susceptible to ingrown toenail complications.
Psoriasis
The condition psoriasis causes orange fingernails is not uncommon. The nails may develop a discolored, chalky substance under the nail that is painful. The nail may also become brittle and split along its length. One-third of people with psoriasis will develop a fungal infection. The yellow-brown color may change to a salmon or orange, and the nail can crumble.
If you’re wondering why your nails are turning orange, it’s essential to know that more than half of those with psoriasis experience nail changes at least once. In some cases, these changes appear years before the joints are inflamed. Psoriasis is primarily diagnosed thorough physical examination and medical history. Blood tests and imaging studies cannot accurately diagnose psoriasis.
The condition can be disguised by using nail hardener and nail polish to hide the symptoms. However, always consult your doctor before applying any products to your nails. To avoid damaging your nails, you should not push the cuticles back or cut them. If you want to clean your nails, you should soak them in warm water to remove buildup. You may want to use unscented products to prevent an allergic reaction.
Two types of psoriasis affect nails: toenails and fingernails. These disorders affect the nail bed, matrix, fold, and hyponychium. In severe cases, the nail plate may separate from the nail bed. During this stage, the fingernail may even fall off. When these symptoms are severe, it’s essential to visit a doctor.
Diabetes
If you’ve been wondering whether diabetes causes orange fingernails, you’re not alone. People with diabetes are more prone to bacterial skin infections, including eyelid sties, boils, and nail infections. Among the most common types of skin infection, diabetes can lead to carbuncles and severe skin conditions. Symptoms of a carbuncle include an itchy, red area that may become swollen or even painful. Treatment for carbuncles contains antibiotics.
The symptoms of onychomycosis are diabetes and yellowing of the nail plate; patients with T2D have thickened toenails. They may also experience edema, a curved appearance, or painful skin along the fold of the nail. In some cases, patients may not seek medical attention until the infection is more advanced. While the condition can take several months or a year to clear up, it is often cured with treatment.
Another symptom is a condition called yellow nail syndrome. Patients with this disease may experience tight or waxy skin in their hands. It may also affect their elbows, knees, and upper back. If the condition is not well-controlled, these symptoms may progress to the other parts of the body. This condition can lead to painful blister-like sores. People with diabetes need to take steps to maintain their blood sugar levels.