What Happens During the Growth Phase of the Nail?

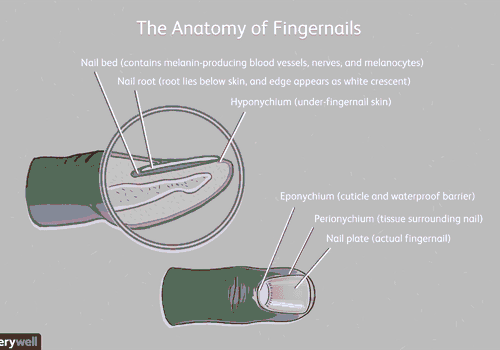
What happens during the growth phase of the nail? The keratin cells at the base of the nail root grow and jostle for space, while older cells edge out from beneath the skin and form the thick, hard nail plate. This plate is pushed forward over the nail bed by continuous division of the matrix cells. If the nail plate grows too long, the nail will eventually break.
Onycholysis
When the nail is affected by onycholysis, the nail plate can no longer attach to the nail bed and will only grow if the underlying condition is cured. However, if the problem continues for more than six months, the nail can permanently change shape and be difficult to grow back up to the original position. This condition is not a severe medical emergency and will usually go away on its own with proper treatment.
The cause of onycholysis is unknown, but certain medications, such as psoralen, are known to induce it. Over-exposure to chemicals, such as those used in manicures, may also lead to this condition. The chemical formaldehyde, a chemical found in nail hardeners, may cause the nail plate to lift. In some cases, fungus infection may also be the cause. In such a case, a person with a nail infection may need to take antibiotics to cure the infection.
The nail will not grow back to its original position in some cases. As the nail grows slowly, the problem will persist until a new pin replaces the removed one. The regrowth time of the nail body/plate is typically four to six months for fingernails and twice that for toenails. Onycholysis is sometimes permanent and can affect the nail’s appearance for life. Therefore, it is essential to avoid trauma to the nails.
Onycholysis is a medical condition characterized by debilitating pain in the fingernail. Blood collects under the nail, and it causes throbbing pain. When the pain persists, a doctor may use a heated needle or a heated wire. This procedure is relatively painless and only takes a few seconds.
Treatment for onycholysis depends on the cause of the problem. The most common cause is a lack of oxygen in the blood. However, it may also be due to a reaction to a medication or trauma to the fingernail. Depending on the cause, the nail body/plate will eventually grow back to its original position. If this doesn’t happen, it is likely to be a symptom of another problem.
Leukonychia

The nail plate may be affected in one or more areas, or the affected area may vary in pattern. It is not related to the reduced calcium content of the nail plate and can be caused by trauma or inflammatory diseases. Although the underlying cause of this condition is unknown, the disease is considered asymptomatic in most cases.
The leading cause of this condition is unknown, but it can be linked to systemic illnesses such as arsenic poisoning, renal failure, and pneumonia. Leukonychia of the nail body/plate is not a life-threatening condition and can be prevented by reducing minor trauma to the nail. However, some forms of leukonychia can be associated with severe illness and should be treated accordingly.
Although white nails are not a cause for alarm, they can be a sign of severe systemic disease or a congenital disease. It is essential to distinguish between leukonychia of the nail plate and the nail bed to diagnose this condition. This article presents information on the various types of leukonychia, their clinical features, and the necessary workup. Once a diagnosis has been made, it will be possible to determine the underlying cause of the white nails.
White nails may indicate a severe illness, so it is essential to seek medical attention immediately. White nails are often a sign of microtrauma to the nail matrix. If the white patches do not reach the edge of the nail, it may be a sign of leprosy, cirrhosis, or typhoid fever. However, they can be caused by trauma to the nail plate.
Affected nails may develop distal splitting in the nail plate. This splitting may be more or less noticeable and maybe highlighted by red bands. The nail plate may also exhibit a ring-shaped white area known as a lunula. In such cases, nail growth may be stunted or ineffective. If this occurs, it may be necessary to undergo a nail-graft procedure.
Koilonychia

A patient with a spoon-shaped nail may simply have an age-related condition. However, this condition may also indicate an underlying disorder, such as hemochromatosis or iron deficiency anemia. A physician can perform a blood test to determine if the patient is suffering from low iron levels and recommend treatment. If a patient has spoon-shaped nails, they should visit a physician.
Physiological onychoschizia occurs when the distal part of the nail plate is damaged by trauma during birth. Parakeratotic cells occupy the plate, impairing transparency and reflecting light. Leukonychia is either transverse or punctate. Transverse leukonychia is rare in children but is common in adults and on the first toenail.
To keep the nails healthy and grow back, the nail bed receives blood and nutrients from the body. The nails grow from the cells at the base nail and layer one on top of the other. The process of keratinization involves the formation of the cuticle (the thin tissue covering the bottom of the nail plate) and the nail plate. These cells push the nail plate forward over the nail bed.
An outgrowth of the nail plate may be caused by a bacterial infection, a virus, or a medical condition. A doctor will perform a thorough examination of the nail bed and hyponychium to identify abnormalities. Ultimately, a new nail will grow out and extrude the remaining part of the old nail. The healing process requires at least seven to 10 days.
When the nail grows back up, the growing portion of the nail is under the skin, at the proximal end. This living portion is called the epidermis. If this part is removed, the nail will grow back to its original position and become stronger and more resilient. But, in some cases, the nail can grow back in a different direction and become disfigured entirely.
A nail body/plate that has undergone surgery is prone to infection. A bacterial infection, such as Staphylococcus aureus, can affect the nail. This bacteria can cause inflammation, pus, and in some cases, conditions. It can also affect the surrounding skin, where the pin is attached. The affected area may be inflamed and have a yellow-green discharge.
Yellow nail syndrome
The condition known as yellow nails syndrome is scarce. Only four hundred or so medical cases have been reported. However, it is not entirely understood what causes yellow nails. Some believe that genetic factors are involved. Some researchers suggest that yellow nail syndrome is inherited in an autosomal dominant pattern, though evidence for this is limited. Autosomal dominant patterns are characterized by a single copy of an abnormal gene. The abnormal gene can be inherited from a new mutation responsible for the disorder. The risk of passing the gene is 50% for each pregnancy and equally for males and females.
Symptoms of yellow nails can be attributed to various conditions, including medications or vitamin deficiency. While there are no known causes of yellow toenails, they are related to an increased risk for infection by toenail fungus. If the symptoms are accompanied by problems in other parts of the body, your doctor may consider yellow nail syndrome to cause the yellowing in your toenails.
If you experience the symptoms of yellow nail syndrome, it’s essential to see a dermatologist for a proper diagnosis. A nail clipping will rule out any fungal elements. Afterward, a physical exam and a detailed clinical history will be conducted. If yellow nail syndrome is the culprit, treatment will be a priority. Patients will need to undergo surgery to correct the problem in some cases.
Although the causes of yellow nails are unknown, researchers have hypothesized that a viral infection could be blamed. These infections usually develop in folds of skin that lie alongside the pin. During this time, the skin may become infected with Staphylococcus aureus bacteria and create a yellow-green discharge. Patients may experience a pronounced pause in nail growth, or the condition may worsen.
In addition to the medical cause, yellow nail syndrome can be caused by a fungus or other underlying condition. A thorough history of exposure can help determine whether yellowing is caused by a fungus or a bacterial infection. However, nail fungus is a contagious disease that affects over 35 million people in the United States. A fungus can be spread through contact with an infected person or skin break.
What Are the Small Ridges in Fingernails?

The most common form of fingernail ridges is a line running from the bottom of the nail to the tip. These ridges indicate aging and affect around 20 percent of adults. Fingernails are made of keratin, the same protein that makes up hair and the outer layer of skin. As we age, our bodies have a more challenging time retaining moisture, resulting in changes in our nails.
Beau’s lines

A nail technician can’t diagnose or treat Beau’s lines. Although a nail technician can offer enhancements to a client with this condition, they can’t perform any type of treatment until they have ruled out any underlying health issues. This condition is typically triggered by exposure to icy environments. It’s best to visit a doctor for a proper diagnosis. Fortunately, there are many treatments for Beau’s lines.
While not as serious as a bacterial infection, ridged nails can signify other problems. Sometimes, they are a sign of systemic issues, such as a thyroid problem, which can affect hormones involved in nail, skin, and hair growth. Other issues with the nails include psoriasis and eczema. In addition to this, people with digestive disorders, such as Crohn’s disease, celiac disease, and ulcerative colitis can develop these lines.
If you have the disease, it can cause Beau’s lines to appear in your fingernails. However, a lack of zinc in the diet can also cause the ridges to appear. People with chronic illnesses that cause an insufficient zinc intake may experience the same condition. This condition can also be a symptom of another disease, including chemotherapy or severe Crohn’s disease.
Although the exact cause of Beau’s lines is not known, it is essential to seek medical attention if you notice a ridge on your fingernails. Unlike other nail problems, this condition usually indicates a systemic issue. Since it affects the growth of claws, a patient who suffers from this condition will experience the same pain on multiple fingers. Therefore, it’s essential to treat the underlying cause if you want to cure your nail infection.
Vertical ridges may be caused by trauma to the nails or excessive exposure to water. A nail doctor can treat these ridges or look for underlying health problems that cause the condition. In some cases, vertical cliffs may also accompany nail bed discoloration. Beau’s lines may indicate a more serious health condition in the most severe cases. Anemia can cause steep ridges in fingernails. Additionally, it can cause changes in the color or texture of the nails.
Splinter hemorrhage

Although the blood vessels of the nail bed are oriented parallel to the axis of the fingernail, a splinter hemorrhage occurs when blood enters the valley between two ridges. This often happens in light trauma or bacterial endocarditis, but other causes can also occur, including cirrhosis and scurvy. If all nails are affected simultaneously, it could be a sign of trichinosis, a disease affecting the thoracic valves in the heart. In addition, some other conditions, such as carbon monoxide poisoning, fungi, or a compromised heart valve, can also cause splinter hemorrhage, resulting in a bright red nail bed.
If you notice small ridges in your fingernails, you may have a splinter hemorrhage. It is a temporary condition that usually does not cause pain. In some cases, however, splinter hemorrhages can become chronic and may require medical treatment. To determine the cause, your physician may prescribe an antifungal or immunosuppressive medication. However, in severe cases, your doctor may recommend surgical treatment or antibiotics to treat the underlying cause.
A reddish rash on the bottom of the fingernails can indicate splinter hemorrhage, a condition caused by a weakened immune system. This condition can also cause brittle nails and signify hematologic disorders. Splinter hemorrhages are not a symptom of a scurvy condition, but they are a sign of infection.
Splinter hemorrhages are caused by the disruption of the blood vessels under the nail bed. They occur most frequently in people with psoriatic arthritis and are often accompanied by white spots on the nails. These spots will eventually grow out on their own. Splinter hemorrhages can also be caused by trauma to the nail bed. Fortunately, most splinter hemorrhages are self-limiting and do not require medical attention.
While it is often difficult to diagnose celiac disease based on the classic symptoms, they signify vitamin C deficiency. If left untreated, these small ridges may lead to severe complications, such as amyloidosis or a lichen planus. However, there are ways to prevent these from happening in the first place.
Punctate leukonychia

Most people assume that vertical ridges in fingernails are related to a vitamin deficiency, but this is not true. In fact, these ridges develop due to minor trauma while the nail is forming. The vertical cliffs will disappear over time, and fingernails will grow for six months. The best treatment for these ridges is using a ridge filler.
There are several types of leukonychia, including transverse, idiopathic, and accurate. These conditions are usually caused by trauma, including shoes and nails, which may break or damage the nail plate. Damage to the thick nail plate may also cause the formation of transverse white bands that move along with the growth of the nail. The treatment for these conditions depends on the underlying cause.
True leukonychia refers to the white spots on the nail plate. It is caused by trauma to the distal matrix. These ridges are composed of parakeratotic cells that impede the nail plate’s transparency, making the nail appear milky white. Leukonychia can also be transverse, which appears as white lines parallel to the lunula.
In contrast, white spots on the fingernails can indicate a vitamin or mineral deficiency. Often, these spots are caused by a lack of calcium, iron, or zinc. A simple solution to the problem is to apply a mixture of mustard oil and neem oil to the affected nails. This oil may also reduce the white spots on the nail plate.
The white spots on fingernails can be caused by minor trauma to the nail plate, such as banging your fingers against a table or door or incorrectly clipping them. However, the damage may have occurred weeks ago and has only become apparent as the nails grow. Other causes for these white spots include exposure to chemicals or poisons, but these are rare. However, you should consult with a dermatologist if you notice white spots on your fingernails.
Although this condition does not have a definitive cure, it is essential to strengthen damaged fingernails and note the symptoms. You may have other medical conditions such as lung problems if you have yellow nails. Punctate leukonychia is caused by various causes, including keratin deposits from nail varnish. In some cases, the reason is an inflammatory skin disease. It may also lead to onycholysis or inflammation of the nail matrix.
Psoriasis

In mild cases, treatment for this condition can include topical retinoid. However, for more severe cases, ultraviolet radiation therapy may be necessary.
The gradual separation of the nail from the skin can cause a pocket underneath. This pocket may be an entryway for fungus or bacteria. The fungal infection may also develop beneath the pin if you have psoriasis. As a result, one-third of sufferers develop fungal infections in their nails. A flaky, chalky substance under the nail may also create. The constant pressure from shoes can cause discomfort.
In addition to using a nail hardener, nail polish may be used to conceal the signs of psoriasis. But always consult your dermatologist before using any of these products. Never pick or push your cuticles because it can cause additional damage to the skin. Picking and removing buildup may also cause infection. To avoid this, soak the nails in warm water after the treatment.
If you suspect that you have psoriasis, visit your doctor right away. They will perform an examination to check whether your symptoms are related to psoriasis. Once diagnosed, you may be prescribed medication to relieve the symptoms. In addition, your doctor may also prescribe medication to treat your psoriasis in general. You should also visit a doctor if you notice that your fingernails have ridges.
Symptoms of psoriasis on fingernails may not be as severe as psoriasis on other parts of the body. Sometimes, however, the nails are the only sites of involvement in the body. Regardless of psoriasis, you may notice small ridges on your fingernails. The pits vary in number and can range from one to several.