Will My Fingernail Grow Back After Acute Paronychia?
If you are suffering from acute paronychia, you are likely wondering, “Will my fingernail grow back?” This article explains the symptoms, causes, and recovery of this condition. It also discusses treatment options. The best course of action for a paronychia infection is to see a medical professional, and if you are unsure, try home remedies before consulting a medical practitioner.
Treatment

Appropriate assessment is essential for the successful treatment of acute paronychia. Several experts are involved, including specialists, medical staff, specialty-trained nurses, and pharmacists. A clinical pharmacist makes sure that patients are following their medication regimen, recommends antimicrobials, and monitors their compliance. A nurse also provides counseling on the medications and reports any adverse reactions to the prescribing clinician.
Acute paronychia may be caused by various pathogens, often staphylococci or staph bacteria. Moreover, a hangnail or trauma to the nail folds can also lead to the infection. Diabetics are at greater risk for developing this condition as the bacteria in their bodies are more aggressive. Some new drugs have also been found to cause acute paronychia.
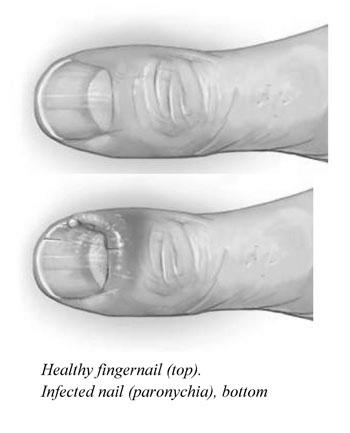
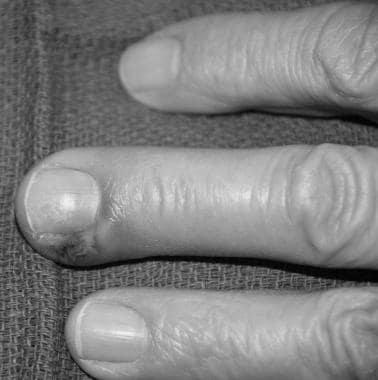
People suffering from acute paronychia should seek medical attention as soon as possible. Symptoms may include swollen or red folds on the nail. The nail plate may also be green or yellow. It will eventually break away from the nail bed. Paronychia can be painful, and a year can pass before it clears up. In the meantime, patients must avoid picking or rubbing their nails, which can aggravate the condition.
In severe cases, incision and drainage are necessary to drain the pus. This procedure can be done in a general practitioner’s office, though surgical units and A&E departments are more likely to perform. Using moist heat on the affected area three or four times per day helps the healing process. Patients should also be sure to change the bandage after one to seven days. The doctor will tell them how long they should leave the application on for optimal results.
A systemic antibiotic against S.aureus may be prescribed in severe cases of acute paronychia. Other antimicrobials that may be prescribed include Ps. and Streptococcus. Flucloxacillin is named four times per day and Clindamycin twice daily for seven to ten days. Surgical intervention may be the only option if these antibiotics do not work.
Symptoms

Appropriate evaluation is the first step in treating paronychia. The patient’s history and physical examination will provide clues about what might have caused the infection. Treatment can then be tailored to avoid complications or worsen the condition. Listed below are some common symptoms of acute paronychia. In addition to the above symptoms, patients may also experience numbness, swelling, or pain in the affected area.
In some cases, herpes simplex virus type 1 is the culprit. In such cases, it may be confused with bacterial paronychia. This form is more common in immunocompromised individuals and health care workers. The infection usually starts as a localized swelling with clear blisters. Viral cultures and serum antibody titers can help determine the infection’s cause. Antiviral medications are often used to treat herpes simplex virus type 1 or 2. Patients should seek medical advice if the symptoms persist.
When these symptoms occur, treatment should be tailored to the underlying cause. Acute paronychia is an infectious disorder of the nail. It can be triggered by excessive hand washing, improper foot care, recurrent manicures, pedicures, or an allergic reaction to nail polish or other wet products. A doctor may order imaging to rule out bone involvement in severe cases. A medical professional will examine the nails for fungus and will advise on further treatment.
Acute paronychia develops in a matter of hours. Herpes simplex causes multiple tender vesicles, and S. causes single or multiple inflamed nail folds. These conditions can lead to fever, tender lymphadenopathy, and even lymphangitis. So, proper diagnosis and treatment will be necessary to avoid serious complications.
If you have any symptoms of acute paronychia, consult a physician immediately. Antibiotics can be prescribed as needed, but only when an extensive infection has been found. In the meantime, a doctor may prescribe an on-site treatment with bacitracin to fight the disease. Patients should follow up with a doctor within 24 hours or 48 hours for the best results. Besides, it is recommended to apply warm water to the affected area for about 24 hours to heal the infection.
Causes

Acute paronychia is a painful, inflammatory disorder of the fold of the nail. In most cases, it is caused by Staphylococcus aureus bacteria, though candida and the cold sore virus can also cause it. Acute paronychia typically develops after minor trauma, such as a hangnail or a manicure. It can be characterized by redness and swelling of the nail fold and pus. Some people have pus expressed from under the cuticle, and others can develop chronic paronychia, which is caused by a mixture of yeasts. People with poor circulation and women are at higher risk for chronic paronychia.
Diagnosis of paronychia is usually made through a physical examination. The doctor will consider your medical history to determine the risk factor(s) involved. They will also collect a pus sample to analyze the condition. Some doctors may use methicillin-resistant S. aureus for psoriasis or pyogenic abscess. However, the treatment for acute paronychia is usually a temporary fix.
If your child has a history of this condition, consider taking precautions to avoid traumatic trauma to the area. Wearing gloves while performing manual tasks may also reduce developing acute paronychia. If the situation becomes chronic, the treatment should be directed towards a fungal cause. Candida species is the primary culprit in chronic paronychia. If the infection is recurrent or difficult to treat, the doctor may choose to pursue other inflammatory conditions of the digits.
In severe cases, the infection may progress to chronic paronychia. The good news is that acute paronychia usually heals in a few days. It can also go to a more severe condition called osteomyelitis. In extreme cases, a person may be prescribed oral antifungal drugs or even a combination of the two. Acute paronychia usually heals within a week or two.
In some cases, the infection may spread under the fingernail. In this case, a physician may remove the fingernail or partial nail to drain the pus. A small blunt instrument is used to elevate the eponychium fold, which allows the surgeon to view the proximal edge of the nail and drain the pus without destroying the matrix. This procedure is a surgical procedure that can be effective and safe for patients.
Recovery

Fortunately, recovery after acute paronychia is relatively simple. Treatment involves warm soaks and topical steroids if needed. In some cases, an abscess may form, requiring drainage. Drainage methods include a hypodermic needle or a wide incision with a scalpel. Oral antibiotics are typically prescribed only when the infection is severe. If you notice swelling, it may be time to see a doctor.
A physician can diagnose paronychia with a physical exam and look for risk factors. Your doctor may also need to collect a sample of pus for testing. The resulting pus can be analyzed in a laboratory. Recovery after acute paronychia will likely include a change of socks and shoes. It’s important not to pressure the infected area for more than two days.
The infection usually starts with redness and generalized swelling in the fingers. Depending on the severity of the disease, a doctor may prescribe a topical antifungal or oral antibiotic. The doctor may also recommend surgical removal of the infected fingernail. Surgical removal of the infected nail may be necessary to prevent abscess formation. For those who have undergone surgery, recovery after acute paronychia may be difficult.
Treatment for chronic paronychia will depend on the pathogens present and local resistance patterns. This condition is characterized by the presence of a fungus or virus in the infected area and persistent symptoms lasting for more than six weeks. Certain nail products, household chemicals, and those used by florists, bakers, dishwashers, and swimmers can all be sources of irritation. Sometimes, aggressive treatments may be needed to restore the protective barrier between the nail and the skin. Recovery after acute paronychia will require several weeks or even months.
The best way to treat paronychia is to avoid recurrent episodes and follow a regimen of antifungal medications. Medications for acute paronychia are usually prescribed by a doctor or dermatologist. However, home remedies may be an effective way to manage the condition and speed up your recovery. However, it is essential to follow the doctor’s advice to avoid complications.
Will My Fingernail Grow Back After Acute Paronychia?

If you are suffering from acute paronychia, you are likely wondering, “Will my fingernail grow back?” This article explains the symptoms, causes, and recovery of this condition. It also discusses treatment options. The best course of action for a paronychia infection is to see a medical professional, and if you are unsure, try home remedies before consulting a medical practitioner.
Treatment

Appropriate assessment is essential for the successful treatment of acute paronychia. Several experts are involved, including specialists, medical staff, specialty-trained nurses, and pharmacists. A clinical pharmacist makes sure that patients are following their medication regimen, recommends antimicrobials, and monitors their compliance. A nurse also provides counseling on the medications and reports any adverse reactions to the prescribing clinician.
Acute paronychia may be caused by various pathogens, often staphylococci or staph bacteria. Moreover, a hangnail or trauma to the nail folds can also lead to the infection. Diabetics are at greater risk for developing this condition as the bacteria in their bodies are more aggressive. Some new drugs have also been found to cause acute paronychia.
People suffering from acute paronychia should seek medical attention as soon as possible. Symptoms may include swollen or red folds on the nail. The nail plate may also be green or yellow. It will eventually break away from the nail bed. Paronychia can be painful, and a year can pass before it clears up. In the meantime, patients must avoid picking or rubbing their nails, which can aggravate the condition.
In severe cases, incision and drainage are necessary to drain the pus. This procedure can be done in a general practitioner’s office, though surgical units and A&E departments are more likely to perform. Using moist heat on the affected area three or four times per day helps the healing process. Patients should also be sure to change the bandage after one to seven days. The doctor will tell them how long they should leave the application on for optimal results.
A systemic antibiotic against S.aureus may be prescribed in severe cases of acute paronychia. Other antimicrobials that may be prescribed include Ps. and Streptococcus. Flucloxacillin is named four times per day and Clindamycin twice daily for seven to ten days. Surgical intervention may be the only option if these antibiotics do not work.
Symptoms

Appropriate evaluation is the first step in treating paronychia. The patient’s history and physical examination will provide clues about what might have caused the infection. Treatment can then be tailored to avoid complications or to worsen the condition. Listed below are some common symptoms of acute paronychia. In addition to the above symptoms, patients may also experience numbness, swelling, or pain in the affected area.
In some cases, herpes simplex virus type 1 is the culprit. In such cases, it may be confused with bacterial paronychia. This form is more common in immunocompromised individuals and health care workers. The infection usually starts as a localized swelling with clear blisters. Viral cultures and serum antibody titers can help determine the infection’s cause. Antiviral medications are often used to treat herpes simplex virus type 1 or 2. Patients should seek medical advice if the symptoms persist.
When these symptoms occur, treatment should be tailored to the underlying cause. Acute paronychia is an infectious disorder of the nail. It can be triggered by excessive hand washing, improper foot care, recurrent manicures, pedicures, or an allergic reaction to nail polish or other wet products. A doctor may order imaging to rule out bone involvement in severe cases. A medical professional will examine the nails for fungus and will advise on further treatment.
Acute paronychia develops in a matter of hours. Herpes simplex causes multiple tender vesicles, and S. causes single or multiple inflamed nail folds. These conditions can lead to fever, tender lymphadenopathy, and even lymphangitis. So, proper diagnosis and treatment will be necessary to avoid serious complications.
If you have any symptoms of acute paronychia, consult a physician immediately. Antibiotics can be prescribed as needed, but only when an extensive infection has been found. In the meantime, a doctor may prescribe an on-site treatment with bacitracin to fight the disease. Patients should follow up with a doctor within 24 hours or 48 hours for the best results. Besides, it is recommended to apply warm water to the affected area for about 24 hours to heal the infection.
Causes

Acute paronychia is a painful, inflammatory disorder of the fold of the nail. In most cases, it is caused by Staphylococcus aureus bacteria, though candida and the cold sore virus can also cause it. Acute paronychia typically develops after minor trauma, such as a hangnail or a manicure. It can be characterized by redness and swelling of the nail fold and pus. Some people have pus expressed from under the cuticle, and others can develop chronic paronychia, which is caused by a mixture of yeasts. People with poor circulation and women are at higher risk for chronic paronychia.
Diagnosis of paronychia is usually made through a physical examination. The doctor will consider your medical history to determine the risk factor(s) involved. They will also collect a pus sample to analyze the condition. Some doctors may use methicillin-resistant S. aureus for psoriasis or pyogenic abscess. However, the treatment for acute paronychia is usually a temporary fix.
If your child has a history of this condition, consider taking precautions to avoid traumatic trauma to the area. Wearing gloves while performing manual tasks may also reduce developing acute paronychia. If the situation becomes chronic, the treatment should be directed towards a fungal cause. Candida species is the primary culprit in chronic paronychia. If the infection is recurrent or difficult to treat, the doctor may choose to pursue other inflammatory conditions of the digits.
In severe cases, the infection may progress to chronic paronychia. The good news is that acute paronychia usually heals in a few days. It can also go to a more severe condition called osteomyelitis. In extreme cases, a person may be prescribed oral antifungal drugs or even a combination of the two. Acute paronychia usually heals within a week or two.
In some cases, the infection may spread under the fingernail. In this case, a physician may remove the fingernail or partial nail to drain the pus. A small blunt instrument is used to elevate the eponychium fold, which allows the surgeon to view the proximal edge of the nail and drain the pus without destroying the matrix. This procedure is a surgical procedure that can be effective and safe for patients.
Recovery
Fortunately, recovery after acute paronychia is relatively simple. Treatment involves warm soaks and topical steroids if needed. In some cases, an abscess may form, requiring drainage. Drainage methods include a hypodermic needle or a wide incision with a scalpel. Oral antibiotics are typically prescribed only when the infection is severe. If you notice swelling, it may be time to see a doctor.
A physician can diagnose paronychia with a physical exam and look for risk factors. Your doctor may also need to collect a sample of pus for testing. The resulting pus can be analyzed in a laboratory. Recovery after acute paronychia will likely include a change of socks and shoes. It’s important not to pressure the infected area for more than two days.
The infection usually starts with redness and generalized swelling in the fingers. Depending on the severity of the disease, a doctor may prescribe a topical antifungal or oral antibiotic. The doctor may also recommend surgical removal of the infected fingernail. Surgical removal of the infected nail may be necessary to prevent abscess formation. For those who have undergone surgery, recovery after acute paronychia may be difficult.
Treatment for chronic paronychia will depend on the pathogens present and local resistance patterns. This condition is characterized by the presence of a fungus or virus in the infected area and persistent symptoms lasting for more than six weeks. Certain nail products, household chemicals, and those used by florists, bakers, dishwashers, and swimmers can all be sources of irritation. Sometimes, aggressive treatments may be needed to restore the protective barrier between the nail and the skin. Recovery after acute paronychia will require several weeks or even months.
The best way to treat paronychia is to avoid recurrent episodes and follow a regimen of antifungal medications. Medications for acute paronychia are usually prescribed by a doctor or dermatologist. However, home remedies may be an effective way to manage the condition and speed up your recovery. However, it is essential to follow the doctor’s advice to avoid complications.