Why Do Nails Go White at the End of Them?
What is the cause of the white nail end? Trauma often causes a white end to the pin. A pink band sometimes accompanies a white nail end on the nail bed. A white half-moon near the nail base is a lunula, Latin for “little moon.” It is indistinguishable from the rest of the nail and indicates that the veins beneath the nail have changed.
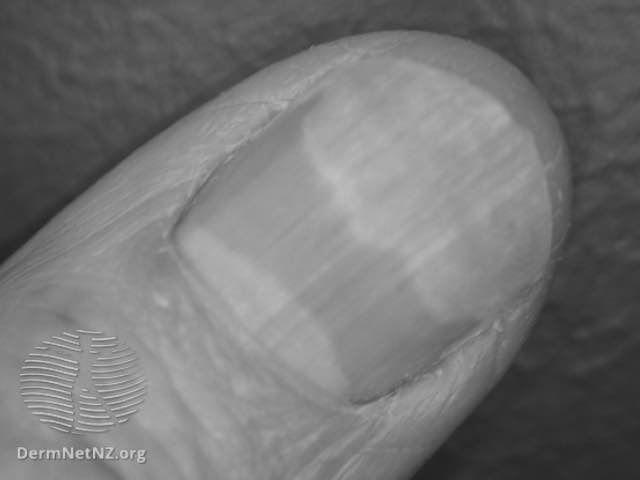
Leukonychia

There are two main types of leukonychia: actual and apparent. In true leukonychia, the white area moves with the growth of the nail plate, while in apparent leukonychia, the white color stays.
The cause of leukonychia is unknown, but it is thought to be caused by several factors. HIV infection, liver cirrhosis, arsenic or lead poisoning, and acute illness are known to cause this condition. Some of these conditions also deteriorate the nail’s health, resulting in white marks and spots.
True leukonychia is caused by arsenic or thallium intoxication. Mees lines are white lines that migrate across the nail’s distal matrix. The lines may appear on one or several fingers. In some cases, these lines can be associated with other diseases, such as Hodgkin’s disease, renal failure, or hypoalbuminemia.
While leukonychia is not generally alarming, it is essential to identify it in time. The condition can mask severe congenital or systemic diseases. However, distinguishing between these two types is necessary for proper diagnosis. Morphological and anatomical classifications of the nail plate are required. , a reliable diagnosis is possible.
While there is no clear genetic cause for true leukonychia, there is a genetic component. Some cases of leukonychia are inherited from a parent. Some mutations in the PLCD1 gene and the GJA1 gene are suspected of causing the disorder; however, exposure to toxic chemicals or a weakened immune system.
True leukonychia affects the entire nail plate. The condition can be hereditary or autosomal dominant, and treatment requires addressing the underlying disorder. In some cases, matrix injury is the cause of the white nail spots. The white areas appear over four weeks. The most common type of leukonychia is a genetic disorder, but an underlying condition may be the underlying cause in other cases.
It is often accompanied by linear erythromycin, a disorder characterized by increased or decreased vascularization. It can also be caused by a benign nail bed tumor or a fungal infection called onychomycosis.
True leukonychia involves the whitening of the entire nail plate. It may be subtotal or total, with the former occurring after local trauma, while the latter may occur as a disorder symptom. If the patient is afflicted with a disease of the nail apparatus, leukonychia should be evaluated as possible.
Microtrauma

Yellow nails are a symptom of an underlying health issue. They turn white at the end is unclear, but the condition can be attributed to several factors. Poor circulation can contribute to yellowing, as can an infection or chronic disease. Some common causes are aging, Raynaud’s phenomenon, and diabetes. In some cases, the condition may also signify a more serious health issue, such as pulmonary embolism.
The condition is caused by an inherited gene and can also be caused by a fungal infection or an allergic reaction to nail-care products. Fungal infection or an allergic reaction to acrylic or gel manicure ingredients are other causes of white spots on the end of the nails. Fungus, bacteria, or a fungus can grow on the nails in a warm, moist environment. A nail-clipping procedure may even cause an infection in some people.
If you are experiencing white fingernails at the end, you should consult a doctor. Having a white nail at the end of your nails can signify an underlying condition, such as heart failure, diabetes, or cirrhosis. You may also notice red or brown lines at the ends of your nails, which is a sign of a heart problem.
The most common cause of nail-whiteness is trauma. A traumatic injury can cause blood under the nail. Although most cases of this condition are temporary, severe trauma can result in a splinter hemorrhage that requires draining by a doctor. A blood clot under the nail may signify a bacterial or viral infection. The condition can also be caused by improper clotting in the blood.
Other possible causes include genetics, autoimmune disease, and chronic kidney disease. In some cases, the underlying condition is related to a person’s anxiety, and the best treatment is to identify and treat the underlying ailment. Dr. Davis typically asks patients about their anxiety levels and refers them to a mental health professional for further diagnosis. If these reasons are not the cause of your white nail problem, consult your doctor.
If the cause is an infection, you can try over-the-counter or prescription antifungal medications. Surgical treatments for this condition can include the removal of the affected nail. If the pin is yellow, you can consult a doctor about other possible causes. It is also important to note that a fungal infection causes the condition, and treatment can include antifungal medications. You may also be suffering from anemia.
Dehydration of keratin molecules

The keratin granules at the ends of your nails are caused by excessive dehydration of keratin molecules. These granules are caused by prolonged wear of nail polish or dehydrating nail polish removers. In some cases, exposure to harsh chemicals such as bleach and acetone can also cause keratin molecules to become dehydrated. The keratin molecules tend to aggregate together and become chalky in either case.
In mammals, keratin filaments form at the ends of the nail. The keratin molecules become filled with glycerol and urea molecules as they age. This process transforms keratin-rich cells into rigid, durable structures. It is also responsible for cuticles, which are thin layers of skin. In human skin, the skin is made up of different proteins, depending on the type of cells.
The core of keratin filaments is blue and contains protruding terminals. This filament is relatively insensitive to changes in hydration. Higher RH values alter the arrangement of chains in intertwined peptide segments. Nonetheless, the terminal parts of the keratin filaments remain rigid, indicating that hydration is the cause of their protrusions.
Dry corneocytes display the most dramatic changes in q position in response to RH. Intact SC and isolated corneocytes also show the same sensitivity to hydration. In addition, these two types of cells are not affected by the lateral packing of lipids in the SC. So, if you have dry, dehydrated corneocytes, or both, you can still get the same results.
A recent study reveals a correlation between interchain distance in keratin filaments and the corresponding molecular dynamics. These results are consistent with previous studies, which suggest that material properties change abruptly at threshold RH. is an excellent example of how RH and water content are linked. The findings from this study have important implications for understanding how our nails function. It also supports the hypothesis that the keratin strands respond to various influences.
What Can Fingernails Say About Your Health?

If you are worried about your health, your fingernails might be telling you something. Pitting, a tiny dent on the nail bed, may signify an autoimmune disorder. This condition is characterized by inflammation and occurs when the immune system mistakenly attacks healthy cells. Pitting on your fingernails can be a sign of various health issues.
Symptoms

If you’re looking for signs of illness, fingernails might be one of the first places to look. Changes in fingernails may indicate several medical problems, including heart disease, thyroid issues, and malnutrition. In addition, the shape and size of your nails may indicate underlying conditions, including diabetes and autoimmune disorders. If you notice any changes in your fingernails, you should seek medical attention.
Healthy fingernails are uniform in color and smooth, free of discoloration or white streaks. If you notice any of these changes, contact your doctor or dermatologist for a diagnosis. Other signs include pain, discoloration, or dark spots under the nail. Also, look for signs of anemia or skin cancer. A health care provider can advise you on the best way to treat a nail disorder or determine if it’s time to get some professional help.
If your fingernails become yellow, they could signify several health problems. Thyroid disease, psoriasis, and diabetes are all symptoms that you should look. Vitamin E and a multivitamin can help fight infection. Another redness on the fingernails may be a splinter hemorrhage. It’s likely the result of trauma to the area.
There are many causes for the yellow color of your fingernails. These conditions may be caused by dark nail polish, smoking, or fungal infection. However, they are signs of more severe conditions when they become thick. The whiteness or discoloration of your nails may indicate a health issue, such as rheumatoid arthritis or a thyroid disorder. If your nails are discolored, you should consult with a medical professional immediately.
Changing nail color is one of the most common reasons to visit a dermatologist. Nail discoloration can signify melanoma, a dangerous form of skin cancer. A dermatologist can identify the condition early and help you avoid any further complications. Fortunately, it is not difficult to prevent the development of melanoma. If you notice any changes in your nails, you should see a dermatologist immediately.
Causes

The health of your fingernails is essential for your general wellbeing. If your nails look discolored or have abnormal shapes, this could signify an underlying medical condition. For example, dimpled nails may be caused by psoriasis, a chronic skin disorder. A deformed or loose nail can be a sign of a thyroid problem. A blue pin could also result from poor circulation, which could signify Raynaud’s phenomenon or another condition. Often, oil drops and salmon patches are signs of psoriasis. Additionally, the fungus can cause these changes in the nail and make them peel and break.
Sometimes, a child’s fingernails may indicate a severe medical condition. At home, a doctor should treat serious infections. Symptoms of the disease can include redness, swelling, pus, and pain. In addition to these symptoms, doctors may also check the fingernails during routine checkups. Having healthy fingernails can provide clues about the condition of a child’s overall health.
Liver diseases such as hepatitis B and C can also cause abnormal changes in fingernails. While diet does not cause these changes, severe malnutrition can. Depending on the severity of the condition, some of these problems can respond to simple lifestyle changes and self-help techniques. Older people are particularly susceptible to developing these problems. Other causes of fingernails for health include injury, infection, trauma, poor circulation, and poor nerve supply.
Changing nail color or texture could signal an underlying medical condition. To find out what is causing the changes, consult a dermatologist. This way, your physician can determine the best course of treatment. For now, it is essential to understand the health risks of fingernails. However, it would help if you didn’t ignore any changes to your fingernails unless you’re sure it’s an emergency.
A white spot near the nail tip may indicate a fungal infection, or a V-shaped nick could be an indicator of a skin disorder, fortunately, by changing your diet. Vitamin B and Zinc can significantly strengthen your fingernails. The problem may be genetic, but a proper diet can help. And a balanced diet is always the best treatment for these conditions.
Signs

While the color of your fingernails might not give away your condition, there are many things that they can tell you. First, your nails should be pink at the nail bed and white at the tip. If they are white or yellow, you might have an underlying medical condition such as a heart problem or lung disease. If you notice these changes, you should visit your physician. Otherwise, you may have an infection.
If your nails are round and have rounded edges, you could be suffering from clubbing. This condition results in your nails becoming swollen and red and can also be caused by a pulmonary disorder. Your fingernails may look a bit dislodged and ragged. It could also indicate an underlying medical condition. It’s essential to seek medical attention if you have a bumpy nail bed.
Your fingernails can also tell you if you have a bacterial infection under them. If you have a cut near the cuticle, bacteria will enter and infect the skin under the nail. The skin surrounding the nail may become inflamed, swollen, and painful. With antibacterial medication, you should visit your doctor immediately if it persists.
Some nail problems are more evident than others. Some people suffer from brittle, split, or yellow nails. The appearance of these problems can be a sign of an underlying health problem, such as anemia. A simple physical exam will help determine whether you’re suffering from a bacterial infection, while others will have nail thinning. A doctor can help you identify the cause of your fingernails by performing a thorough exam.
If you want to learn more about the body parts that affect your fingernails, check out the information below. Many people don’t realize that their fingernails can give them some insight into the health of their entire body. Moreover, many of the changes in fingernails are harmless and are part of aging. In some cases, they may also be a side effect of certain medications.
Treatment

Your fingernails are a vital part of your health and appearance. They protect your fingertip tips and skin and help you peel an orange or scratch an itch. Typically, your fingernails should be smooth and uniform in color without discoloration. However, if you notice any changes in your fingernails, you should immediately see a dermatologist, health care provider, or doctor. Common signs of a health problem include discoloration, pain around the nails, and white spots under the nail.
If your fingernails show minor dents or ridges in the nail bed, you may have psoriasis-related blood type-related conditions. Extra hormones coursing through the veins can affect your nail growth during pregnancy. You may also experience pain or discomfort when walking. The symptoms of nail psoriasis are similar to symptoms of psoriasis.
Nail ridges and streaks, known as Muehrcke’s lines, are common signs of severe health problems. They can indicate an underlying condition, such as anemia or hemochromatosis. Fortunately, a good diet includes many vitamins B and zinc. However, it’s recommended to see a physician if your fingernails are becoming discolored, as these ridges and streaks indicate a more significant problem.
Occasionally, nail changes are a sign of underlying problems. If you pick at your fingernails or use harsh chemicals or hair dyes, you increase your infection chances. Likewise, picking at your nails can cause infection and damage your teeth. Other causes of nail problems include injury, illness, disease, and poisoning. A dermatologist can determine the cause of the problem.
Liver problems may be responsible for fingernail problems. Liver cirrhosis and hepatitis B and C can all lead to fingernail issues. In a 2010 study, researchers compared 100 patients with liver diseases to 100 healthy volunteers. They found that 68 percent of the liver patients had changes to their fingernails. In contrast, only 35 percent of healthy subjects showed any changes. Nail fungus, horizontal ridges, and brittleness were common in these patients.