How Diseases Affect Our Nails

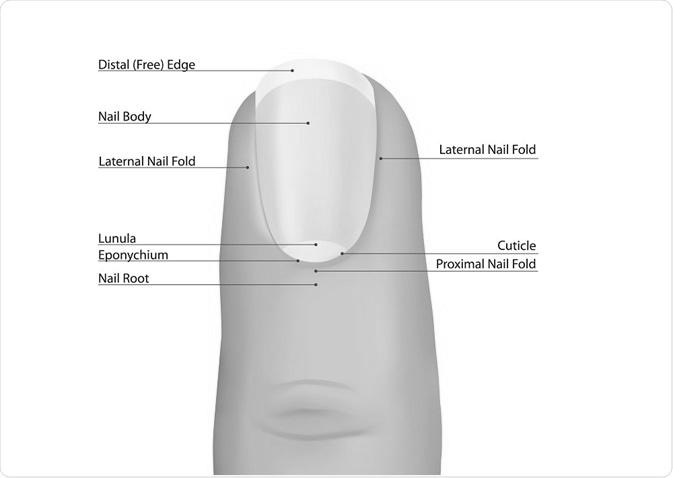
According to Dr. Purushottam Vashistha, a consultant gastroenterologist at Nanavati Super Speciality Hospital in Mumbai, the health of the liver and gastrointestinal tract can affect our nails. In some cases, poor nutrition or absorption can result in flat, concave, or whitish nails or the disappearance of the lunula. The pins are excellent diagnostic tools, so they should not be overlooked.
Beau’s lines

There are various types of nail disorders. The most common is onychomadesis, affecting about 25% of the population. Exposure to radiation and chemotherapy may also cause Beau’s lines.
The onset of Beau’s lines is an indicator of a systemic illness or drug reaction. Although they may appear as deep indentations in the nail plate, they are transient and will grow out with continued nail plate growth. Treatment of this disease must address the underlying systemic abnormality. Fortunately, there is no specific treatment for Beau’s lines. In many cases, however, additional treatment may be necessary.
Several other nail diseases can cause Beau’s lines. One of the most common is onychomadesis, which is the proximal separation of the nail plate from the nail bed. Acute eczema can cause a similar condition, inflaming the nail area. For example, an athlete may develop Beau’s lines after running for long periods.
Leukonychia

White discoloration of the nails is a fairly common condition, but it can mask more serious underlying conditions, including liver and kidney failure. As such, a reliable assessment is crucial to identifying the underlying cause. This article reviews data on several leukonychia types, their clinical features, and pathogenesis. It also discusses the necessary workup for these patients. To help you understand how to diagnose leukonychia, we will discuss its classifications, clinical features, and treatment.
The symptoms of leukonychia and other nail diseases may include white discoloration of the nails or lines. These lines are paired bands parallel to the lunula and are most common on the second, third, and fourth fingernails. Biopsies are necessary only for true longitudinal leukonychia, nail lichen planus, and Darier disease.
A genetic linkage study has revealed a possible connection between leukonychia and the PLCD1 gene. The PLCD1 gene is located on chromosome 3p22-p21.3. Although the cause of leukonychia is unknown, some individuals with the condition may inherit the gene from their mother. Other factors can also cause the disease. In rare cases, it may also occur due to radiation therapy.
Koilonychia

While koilonychia is not a disease, it is a symptom of an underlying condition that can be very dangerous. If it is not treated, it can lead to systemic and dermatological problems. The best course of treatment depends on the underlying condition and can range from behavior modification to surgery. If koilonychia is severe, a dermatological consultation may be necessary.
A thorough workup is essential to rule out underlying cutaneous disorders and differentiate between different aetiologies. In addition, most acquired koilonychia causes are reversible, making them a good choice for newborns. Newborn nails are often soft and thin, so a wait-and-watch policy should be used for these babies, and parents should be encouraged to observe the condition closely and seek medical attention if it persists.
People with koilonychia often have nail problems caused by iron deficiency or fungal infections. Iron-deficient diets can also lead to nail changes. Vitamins A and C can help increase iron absorption. If these treatments are not successful, a doctor may prescribe medication. A healthy diet can improve the condition and heal the nail. A full regrow of fingernails can take 6 to 18 months.
Paronychia

Acute paronychia is a painful bacterial infection that can appear on the fingernails or toenails. It often results from a broken nail, prick from a thorn or splinter, or any other type of skin break. Pathogens most likely to cause acute paronychiae are Staphylococcus aureus and b-hemolytic streptococcus. It can cause infection and swelling, and secondary pus may form. The nail matrix is particularly fragile in children, leading to permanent dystrophy.
Paronychia is often associated with underlying medical and skin problems. It can be acute or chronic and affect a single finger or several fingers. Pain and swelling may occur around the nail in the early stages, and a pus-filled pocket may develop. The nail plate may erode, break down, or become thick in chronic paronychia.
Inborn children, koilonychia (thick, big toe, and thumb) is often caused by a bacterial infection. While the disorder is generally benign, it can be associated with several other skin diseases. There are no known treatments for this disorder, but they can be treated in some instances.
Symptoms of melanoma

One of the many ways melanoma can appear on our skin is in the nails. In some cases, nail melanoma can take the form of a bump or nodule under a fingernail. Other times, it can take the form of a new dark band on a nail. Nail melanoma is more dangerous than skin melanoma, and it is essential to seek medical attention for any suspicious changes.
Most cases of subungual melanoma are characterized by a brown or black streak in the nail bed, which may progress to thickening and splitting of the nail.
Although nail melanoma is more common in the big toe and thumbnail, every nail bed has a chance of developing the disease. However, in a UK study, only 1.4% of patients had the disease in their nails over 10 years. Of those who grew NUM, only 51 percent survived the five-year follow-up period. However, the treatment of melanoma in the nail unit is complicated, requiring a biopsy of the affected nail matrix and nail bed.
Onycholysis

Onycholysis is a condition that occurs when the nail plate separates spontaneously from the nail bed at the proximal, lateral, and distal free margins. It most commonly occurs in psoriasis of the nails and is also known as onychomadesis. Physicians may use topical corticosteroids, pulsed-dye laser treatments, or psoralen plus ultraviolet A therapy to treat onycholysis.
The presence of fungi on the nail can indicate a bacterial, fungal, or viral infection. If this condition occurs in just a single nail unit, it is likely secondary to an underlying tumor. However, nail clippings containing fungi and yeast can be sent for histologic analysis to determine whether a fungus or yeast is the cause. Yeast can be a secondary problem, and a primary diagnosis is required to rule out a tumor.
If you’ve noticed a sudden change in the shape or size of your nails, you should consider seeing your doctor. An oncolytic pin can be caused by an underlying condition, but the fungus or yeast infection can be cured using oral prescription medicine. These medications are expensive and often not covered by insurance. However, onycholysis should not be treated without consulting a healthcare provider, who may prescribe a different treatment based on the symptoms and the underlying problem.
COVID-19

Although there is no specific treatment for COVID-19 infection, early diagnosis is crucial.
Some nail changes from COVID infection are visible, including the development of Beau’s lines. These lines may appear between four and five weeks after the onset of COVID infection. The distance between these lines and the nail base is the key. There is no specific treatment for these lines, but they tend to grow out when the underlying disease has cleared. However, nail changes associated with COVID may take longer to resolve than other COVID symptoms.
This disease does not cause nail thinning, but it does cause irregularities in nail growth. The state can also be accompanied by a ring of pain in the fingernails.
Causes of Peeling Skin Below Finger Nails

Dry skin can cause peeling skin below fingernails. Try using a hydrating agent on the affected area to alleviate this problem. One solution is honey, a natural humectant that attracts moisture from the environment. Simply apply honey to the affected area with a cotton ball and let it sit for 30 minutes. Rinse thoroughly with cold water. If love doesn’t work, petroleum jelly may help. However, be careful with petroleum jelly as it will make the skin feel oily and greasy.
Mild iron deficiency

You might have noticed peeling skin beneath your fingernails. Peeling skin can be caused by various things, including exposure to chemicals, wearing acrylic nails, and even mild iron deficiency. This condition can be caused by multiple underlying health conditions, but the most common cause is iron deficiency. Peeling skin can also be caused by prolonged exposure to UV rays, severe underlying health problems, or a vitamin deficiency. Peeling skin under the fingernails may be caused by an underlying condition, such as anemia or a vitamin deficiency.
A lack of iron may also cause your nails to become brittle and peel. It can also cause restless leg syndrome, nine times more common in iron-deficient people. Another symptom of iron deficiency is brittle, spoon-shaped nails. While these symptoms are not necessarily indicative of iron deficiency, they are signs of this condition.
Apart from peeling skin under the fingernails, mild iron deficiency may signify other health problems. A brittle nail is often a symptom of koilonychia, characterized by brittle fingernails. If you notice peeling skin beneath fingernails, you should visit your doctor immediately. A blood test is needed to check your iron level.
Eczema

Skin peeling beneath the fingernails may be a symptom of an underlying medical condition or environmental factor. Whether you’re exposed to harsh chemicals, too much hand washing, or simply exposing your fingers to extreme weather can cause your skin to peel. If you’re prone to dry skin, frequent hand washing can make your skin dry and prone to infection. Here are some other causes of peeling skin beneath the fingernails.
A deficiency of vitamins and minerals can cause your fingertip skin to peel. If you have dry skin, you may also suffer from eczema. Symptoms of this skin disorder may include dryness, cracking, and scaling. If you’ve noticed peeling skin below fingernails, you should seek medical attention to prevent further complications. While several treatments are available, your doctor may prescribe a topical or systemic medication to cure your condition.
A fungal infection is another possible cause of peeling skin. Tinea is a fungus that typically starts on the palms and gradually spreads to the fingertips and back of the hands. Symptoms may include red rash-like sores and skin that peels off in flakes. Atopy, chronic eczema, and specific vitamins and supplements may also cause the skin to peel.
Dyshidrosis

Dyshidrosis and peeling skin under the fingernails are two conditions associated with the development of sweat glands. The resulting skin rash may be mild or severe, affecting one or more body areas. The blisters will typically appear on the sides of the finger or palm and may eventually merge into more extensive lesions. Symptoms usually resolve within three weeks, but they may reoccur regularly for months or even years.
There are two main types of dyshidrotic dermatitis, with the more severe forms involving the hands. The most potent type is called pompholyx, and it develops as vesicles coalesce into larger masses known as bullae. This skin condition is often treated with topical corticosteroids and lubricant creams, but symptoms can persist even with effective therapy.
If the condition persists or worsens, it may be a bacterial or fungal infection. Excessive hand washing can impair the skin’s lipid barrier, and soap can penetrate the uppermost layers of the skin. Skin that is cracked and peeling can be a sign of various skin disorders, including psoriasis, a chronic inflammatory disease of the hands. In some cases, peeling skin can also be caused by an allergic reaction to a topical irritant or allergen.
Various conditions can also cause the skin to peel around the fingernails. The most common of these are eczema, psoriasis, and dyshidrosis. Psoriasis, for example, attacks the life cycle of skin cells. In contrast, dyshidrosis, which affects sweat glands, results in fluid-filled blisters on the sides of the fingers.
Hydrocortisone
When treating peeling skin below fingernails, you may use hydrocortisone lotion or cream. When applying hydrocortisone lotion or cream, ensure that you wash your hands thoroughly. The medication can irritate the skin if it gets in your eyes, nose, or mouth. Wash with plenty of water after applying it, and contact your doctor if it causes irritation or worsens. Use hydrocortisone only for the condition it’s prescribed for. Don’t use hydrocortisone for more than two or three days, and never use it for more than directed. Also, consult your doctor for the appropriate dosage for children.
There are two main types of hydrocortisone for peeling skin: creams and ointments. Ointments cover the skin with a smooth layer of the active ingredient. These are easier to apply and remove with water. Lotions spread over the skin more smoothly. Sprays are beneficial if you don’t want to rub your skin while using hydrocortisone cream or ointment.
Aside from being a prescription-only medicine, hydrocortisone for peeling skin below the fingernails has several side effects. While it can provide symptomatic relief, it’s not recommended for children under 12. Hydrocortisone is not recommended for use in burns because it can absorb into the skin, making it useless. However, it’s an excellent product for treating peeling skin below fingernails.
Vitamin or calcium deficiency

If you’ve noticed that the skin beneath your fingernails is peeling, you might have a vitamin or calcium deficiency. While calcium is not the only nutrient that can cause brittle nails, it’s essential to pay attention to your nails. Not enough calcium can lead to brittle nails, and your nails may be more susceptible to injury than you realize.
Getting enough vitamin D can help treat peeling skin below your fingernails. Some sources of vitamin D include fatty fish (swordfish and salmon have a high vitamin D content) and fortified foods such as milk and yogurt. In addition to eating vitamin D-fortified foods, you should spend some time in the sun twice a week. However, be sure to use sunscreen while exposing your skin to the sun.
Dry skin can be caused by fungal infections. Candida albicans and dermatophytes are common culprits of fungal infections around the nails. Psoriasis, a chronic skin disorder, can also peel skin around the fingernails. If you lack vitamin D, it can lead to muscular weakness and poor bone density. Peeling skin around fingernails can result from external trauma, including prolonged exposure to water.
White spots on the skin beneath fingernails can signify a zinc deficiency. A zinc deficiency can be easily remedied by allowing your nails to grow. Half moons at the base of your fingernails generally do not cause concern. However, if you notice them becoming red or irritated, consult with a healthcare professional to determine the cause of the peeling skin. Then, apply lotions containing alpha-hydroxy acids or lanolin.
Dehydration

The skin under the fingernails may peel because of dehydration, which can result from weather conditions or simply a lack of moisture. Applying moisturizer is essential for dry skin, and there are a variety of home remedies for peeling skin below the nails. Try hydrating your hands throughout the day and wearing gloves to minimize the chances of a skin infection.
The most common way to treat dehydration is to drink more water. If the condition is mild, you can take a few more glasses of water each day, but if it gets worse, you should visit a doctor. You may need intravenous fluids at a hospital or doctor’s office in severe cases. However, dehydration may be more challenging to treat if the condition is caused by dehydration. Keeping your skin moist is especially important during the colder months, and you should take extra precautions to avoid dehydration.
Insufficient water can cause your skin to become dull, uneven, and wrinkled. Light pinching of the skin can detect dehydration. In severe cases, you should seek medical care, but there are a few home remedies you can try to improve your skin’s health.