What is Nail Infection?

Fungus is a common condition of the skin and nails. Most fungus people get it on their big toenails, on the side or front edge. It is less common to get fungus on the nail base, especially in people with low immune systems and serious illnesses. Fungi that infect the skin are known as dermatophytes or yeast. If you are unsure of nail infection, you can read more about its symptoms in this article.
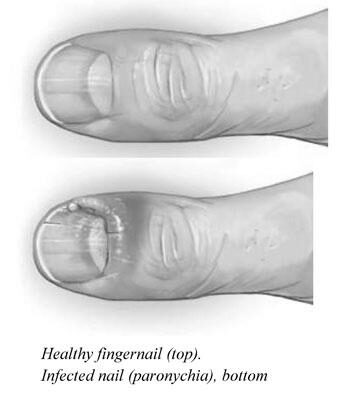
Paronychia

A doctor may suspect a nail infection when a patient has a painful, inflamed fingernail. They may perform a thorough physical examination and take a detailed history to confirm the diagnosis. The past can help determine if other triggering factors have caused the paronychia. Taking the proper treatment can help prevent complications and worsening the infection. Listed below are some ways to treat a paronychia nail infection.
An excellent way to prevent a paronychia nail infection is to avoid manipulating fingernails and frequent hand and foot washing. This prevents fungi, allergens, and skin irritants from penetrating the nail plate. Wearing a pair of cotton gloves is also an effective way to avoid an infection. Finally, wear waterproof gloves to protect the hands and nails from the moisture that can irritate the skin. Once you’ve noticed signs of paronychia, see your healthcare provider as soon as possible.
Treatment for paronychia will depend on the type of infection. If left untreated, it may spread through the blood and bone of the finger. Your doctor may recommend surgery to remove the affected area in severe cases. However, if you think your symptoms might be caused by a yeast infection, you should see a doctor for a diagnosis. Your doctor will take your medical history and examine your finger for a pocket of pus. They may also ask about your profession and how often you get manicures. Blood tests will not be needed in diagnosing a paronychia nail infection.
Treatment for acute paronychia often includes soaking in warm water, consider a simple home remedy. You may also want to consider cutting open the affected nail fold to drain the pus and then placing gauze over it to prevent a recurrence. Once treated, the infection usually clears within a week or two. Then, you can return to your normal activities. You can also follow the same treatment regimen as for acute paronychia.
If you do not treat your paronychia nail infection, the symptoms will worsen. It may develop ridges, waves, or greenish color and can become dry and brittle. It may even detach from the nail bed if not treated promptly. Traumatic events or accidents that damage the nails are the most common causes of paronychia. People who get regular manicures are also at risk for paronychia nail infection.
In addition to medications for acute paronychia, patients may need to follow a strict skincare regime to prevent a recurrence. Treatment for chronic paronychia involves using topical corticosteroid ointments with an antifungal agent.
Onychomycosis

Onychomycosis affects both children and adults but more often occurs in older individuals. The infection is also common in infants, as the nail provides a portal of entry for the fungus. A person may experience social problems, such as embarrassment, due to the condition. People with the disease should seek medical advice immediately and follow any instructions or suggestions given by their doctor.
To diagnose onychomycosis, a physician should evaluate the patient’s nail health. Symptoms may include nail thinning, discoloration, lifting, or crumbling. The condition is highly treatable, but treatment is expensive and may take months or even years. Some patients will show no symptoms for months or may have partial improvement even after receiving antifungal medication.
Onychomycosis is characterized by wide variation in the fungi that cause the condition. It can mimic other diseases, including psoriasis, nail trauma, and infections caused by bacteria. Fungi causing onychomycosis cause 60 to 70 percent of onychomycosis infections. Other opportunistic fungi may also cause the disease.
The infection begins as a white or yellow spot underneath the nail’s tip. If left untreated, the nail may become crumbly or break off entirely. Treatment for onychomycosis will include self-care measures and the application of topical antifungal medications. While the condition can be treatable with self-care measures, it is often reoccurring. If the infection is severe, the patient should seek medical attention immediately.
After taking a swab from a fingernail or toe, the specimens were disinfected with 75 % ethanol. Yeasts were previously thought of as colonizers and contaminants but have now been recognized as pathogens in nail infections. In fact, they are also known as non dermatophyte fungi. Onychomycosis’s clinical signs and symptoms vary widely from one person to another.
Onychomycosis is often challenging to diagnose because of traditional methods’ lack of sensitivity and specificity. Despite this, commercial real-time PCR can detect dermatophytes in nail samples. In fact, qPCR provided an etiologic diagnosis in 55.2% of cases, while culture was only successful in 38.1% of cases.
Toenail fungus is a common fungal nail infection. It is caused by fungi or yeast, and it is caused by various factors. It grows under the growing portion of the nail and spreads up the finger, along the nail bed, and into the side grooves. The condition is usually more common in older people and diabetes patients. Onychomycosis can be painful and may impair walking.
Onycholysis

Onycholysis is a condition in which the nails thicken and develop an irregular border between a pink and white edge. The nail plate may be discolored or white, or the entire nail may be opaque. The skin under the nail may also be thickened and discolored. Your doctor will also look for other health problems such as thyroid disorders or skin rashes. Your doctor may also scrape the tissue beneath the nail plate and test the samples for fungus.
While onycholysis is a temporary condition, it can lead to more severe health complications if left untreated. If you don’t take care of the underlying cause of onycholysis, you could cause further damage to your nail and make it impossible to reattach it. In some cases, onycholysis is so severe that the nail bed becomes permanently disfigured and may require surgery.
Onycholysis is characterized by thick, coarse debris usually covered with sparse hyphae. The presence of these hyphae suggests that the etiological agent is a fungus. However, an in vitro laboratory culture is required to identify the exact agent. The specimen should be divided into two parts for microscopy and culture. Unfortunately, direct microscopy does not differentiate between the various pathogens, and there is a substantial chance of false-negative results.
There are different types of treatment for onycholysis. In the long term, oral prescription medicines can help. However, they can be expensive and are often not covered by insurance. If you notice any changes in your nail, you should consult your healthcare provider. The changes are often temporary, but they can take months to disappear. However, it is essential to follow up with your healthcare provider if they persist or if you notice symptoms.
Treatment for onycholysis has varied throughout the ages. Some of the earliest remedies were topical agents, such as imidazoles and allylamines. However, these drugs are ineffective against fungal infections of the nail due to their inability to penetrate the entire nail unit. Systemically-active drugs have been developed in the last few years that can penetrate the whole nail unit.
The incidence of onychomycosis varies, but a recent study University of Iowa found that about 2 to 3% of the general U.S. population is affected by this condition. Those who develop this infection are prone to work impairment and often take time off from work to treat it. Some treatments are effective, but others may be ineffective, leading to patients abandoning treatment. If this happens, they can become permanently disfigured.
Paronychia is an infection of the skin surrounding the nail. There are two types of paronychia: acute and chronic. The acute form is characterized by a yellow-brown ‘oil spot’ and can be pathologically related to psoriasis. A chronic paronychia occurs when the cuticle is damaged over time, and fungi can flourish in the inflamed area. Keeping the skin dry and clean is the first step in therapy, but sometimes antibiotics are needed.
Why Are the Sides of My Nail Yellowish?

If you’re wondering, “Why are the sides of my nail yellowish?” you’ve come to the right place. Below are three possible causes of nail discoloration, plus some helpful tips. If you’re not familiar with these conditions, please read our articles on Onychomycosis, Psoriasis, and Thyroid disease. If none of these causes seem to apply to you, read on.
Onychomycosis

Some medical conditions, such as fungal infections, can cause the sides of your nails to become yellow. These diseases are caused by an accumulation of debris underneath the pin and the thickening of the nail. Treatment requires systemic medication for three to six months. There are also several causes of nail discoloration, including underlying health conditions such as thyroid disease and diabetes. To know the correct diagnosis, consult a dermatologist.
In many cases, yellow toenails are caused by a fungal infection. This type of infection is more common in men than in women, and you can contract it from sharing shoes or broken skin. Another common cause is wearing dark socks or shoes that contain artificial dyes. Other factors that can contribute to yellowing the toenails include diabetes and psoriasis. Furthermore, some injuries can also cause fungus to penetrate the nail.
Smoking is a common cause of discolored nails, but other reasons are. The tar and nicotine in cigarettes can discolor the nails. The best way to prevent yellow nails is to avoid smoking altogether. If you are concerned about your nail color, consult your doctor, as this could be an early sign of a more serious health problem. Common conditions include thyroid disease, liver disorders, diabetes, and lung disease.
Although the exact cause of yellow nail syndrome is unknown, some cases are sporadic and may even be related to another condition. While most cases of yellow nail syndrome are broken, some experts say the disease can be caused by a mutation of the FOXC2 gene. If this is the case, patients with yellow nails are advised to seek medical attention. If there are respiratory symptoms or underlying edema, treatment should be sought as soon as possible.
A healthy nail should be pink at the base of the nail and clean white at the tip. If the sides of your fingernail are yellow, it could signify a fungus infection. This infection is caused by microscopic organisms and causes discoloration. The fungus does not cause pain, but it can cause embarrassment because of its appearance. It is best to see a dermatologist if the discoloration persists or becomes worse.
If the infection is caused by a fungus, it will need systemic medication for three to six months to completely eradicate the disease. The cure rate with current antifungals is 50-60%. Repeating the course of drugs may not completely eliminate the infection. A dermatologist can culture your fingernails to determine the type of fungus. A dermatologist can then prescribe a treatment that combats this fungus explicitly.
A bacterial infection of the nail can also cause discoloration on the sides. This condition is called paronychia and can affect the nail and surrounding skin. Common symptoms include redness, inflammation, and pus around the nail. Additionally, the nail can become thicker and yellow. If you notice this discoloration, you should consult a podiatrist for treatment. If the discoloration is caused by an autoimmune disease, it is best to get it treated immediately.
Psoriasis

If you’re like many people, you may wonder what causes psoriasis to make the sides of your nails yellow. The condition is caused by an overgrowth of skin cells under the nails. As a result, your nails may look yellow or thick. It can even lead to the development of pits. You can minimize the trauma to your nails by keeping them short. This will help prevent them from lifting off your fingers and discourage buildup under them.
You can get fungal infections at the same time that you have psoriasis. Those with fungal infections are at a higher risk of getting the disease. In addition, certain medicines may cause the condition to worsen. Fungal infections are caused by trauma to the nail bed, such as pressure from shoes. Another common cause is a cold sore virus. Lastly, some medicines may make the sides of your nails yellowish.
Removing these cells is painless, but it is essential to remember that this pocket can become a pathway for infection. One-third of all people with nail psoriasis will eventually experience a fungal infection. The nail can become discolored and even crumble if the disease becomes untreated. In addition to the discoloration, the condition can cause the nails to become thicker and more painful, which can cause a fungus to grow underneath.
The treatment of psoriasis can include oral medications such as cyclosporine. A doctor may prescribe a biologic agent such as methotrexate for more widespread nail involvement. In addition, intralesional Kenalog injections may be given to patients. Both types of treatment can help treat the underlying psoriatic arthritis. In some cases, the disease can lead to psoriatic arthritis.
An excellent way to prevent nail psoriasis from worsening is to keep your nails clean and well-maintained. You should file them down and keep them clean. Also, try not to pick them or bite them. To prevent further damage, use a moisturizing lotion. Do not use sharp objects to clean your nails, as this can lead to lifting and infection. Lastly, you should avoid artificial nails and stick to your natural nails. If you must wear fake nails, consider lightly buffing them or using nail polish on them.
Although it can vary from person to person, it is generally not uncommon for psoriasis to affect the sides of your nails. It can look like a fungal infection when it involves the nail plate. Psoriasis may also cause nail fungus or onychomycosis. If you notice your nails become yellow and brittle, consult a dermatologist about treatment.
Thyroid disease

If you’ve ever wondered why the sides of your nail are yellowish, you may have hypothyroidism. Thyroid hormones control metabolism, the process by which we convert our food into energy.
Hair loss, skin loss, and yellowish nails can be symptoms of an underactive thyroid and can be treated with prescription medication. However, if you’re experiencing these symptoms consistently, you may have a thyroid problem. A thyroid hormone test is recommended to determine the cause of the problem and determine the proper treatment. Some labs measure only the thyroid-stimulating hormone. Your lab should measure free triiodothyronine (T3) and thyroxine (T4) to properly diagnose your thyroid condition. TPO antibodies are also used to measure thyroid function.
While many people think of psoriasis as the primary cause of yellow nails, other reasons are more serious, such as iron deficiency or pregnancy. Generally, however, an unhealthy thyroid will result in yellowish sides of the nail, a symptom of a more severe condition. While you should seek medical attention for any unusual appearance of your nails, it’s essential to take the time to check them to make sure they’re healthy and free of any abnormalities.
Thyroid disease affects all of our bodily functions, including the skin. Skin, hair, and nails are some of the first places a clinician will notice symptoms. Your doctor can treat these symptoms with the appropriate medication, but it’s also important to note that it’s essential to consult a dermatologist for a diagnosis. If your symptoms are present, it’s crucial to get a thyroid test to confirm your condition.
Other common causes of yellow nails include vitamin deficiency, psoriasis, and thyroid disease. Yellow nails may signify severe health conditions, such as diabetes, kidney disease, and liver disease. Your doctor will check to ensure no extreme conditions are causing your yellow nails. They’ll be able to rule out other possible causes and recommend a course of treatment.