- What Causes a Green Nail Bed? How Can it Be Treated?
- Onycholysis
- Pseudomonas aeruginosa infection
- Candida parapsilosis
- Why Would a New Toenail Grow Under a Healthy Toenail?
- Ingrown toenails are caused by improper trimming.
- Toenail fungus causes debridement.
- Improper trimming
- Toenail fungus causes dermatophyte fungus.
- Ingrown toenails pose a health risk.
What Causes a Green Nail Bed? How Can it Be Treated?

A green nail bed is caused by bacteria. This bacteria can grow and envelope the entire nail, spreading to other nails and even body parts. Nail polish will only cover up the green nail. Medical treatment is required. If you have any questions about a green nail bed, contact East Carolina Dermatology and Skin Surgery, PLLC, for a consultation.
Onycholysis

You may have onycholysis if you notice your nails have become green or have a discolored edge. A blood test may reveal an underlying cause of vitamin deficiency or thyroid disease. Your doctor can then prescribe appropriate medication to treat the underlying problem. However, until a diagnosis is made, you should treat onycholysis at home with natural remedies. Cleansing beneath the nail can sweep bacteria deeper, causing the problem to worsen. Tea tree oil is an excellent treatment for fungus and yeast infections found beneath the claw. Be sure to dilute any essential oils before applying them to your skin.
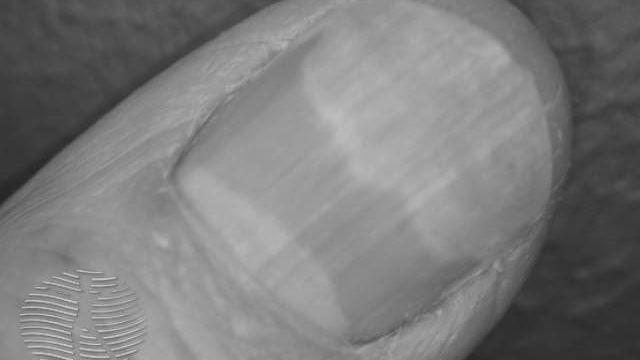
Onycholysis is a condition in which the nail plate separates from the bed, often at the free margin. The area remains white due to air, but it turns green or brown if bacteria colonize the site. Symptoms may first appear in one or more fingernails, such as if a person frequently works with their hands in public. Onycholysis in toenails is almost exclusively the result of trauma. However, if it appears on just one digit, a doctor may suspect a toenail tumor.
Nonprescription medications for onycholysis include ciprofloxacin 500 mg twice daily. It is important to note that oral prescription medicines have potential side effects and may interact with current medications. Patients with onycholysis may try topical treatments such as ketoconazole cream as an alternative therapy. Nail avulsion has been used successfully but should be used only as a last resort.
If associated with longitudinal red and white streaks, it is also known as Darier disease. If you have discoloration in your nail bed, your doctor may recommend a blood test to confirm the diagnosis.
In one case, a 39-year-old man presented with a chronic onycholysis of the middle to the distal part of his left thumb. He denied having undergone any trauma and said he used to go swimming.
Based on your clinical presentation, whether you’ve developed onycholysis is not easy to determine. Various bacterial and fungal infections can cause green nails. In some cases, a combination of both can be the culprit. If you suspect a bacterial or fungal infection, culture your nails in white vinegar and use an appropriate antifungal or antibacterial agent to treat the disease. If all else fails, you can try prescription antifungal medication.
Pseudomonas aeruginosa infection

A Pseudomonas bacterial infection causes a green nail bed. The bacteria produce a pigment called pyocyanin, which inhibits the growth of other bacteria. Predisposing factors include onychomycoses and diabetes mellitus. The organism is also transmitted through wounds and can lead to systemic complications in immunocompromised patients.
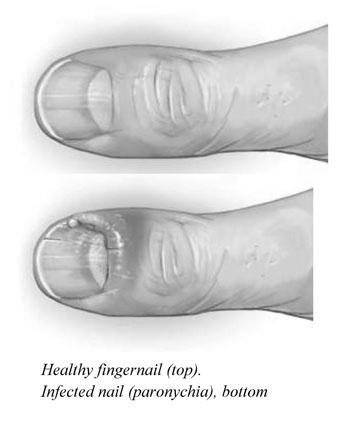
The infection is usually not painful, but the client should visit a physician if the condition becomes painful or starts to produce pus. Antibiotic treatment may be necessary if the infection is mixed with another bacterium, such as adenovirus. A physician may drain the infected area or culture the bacteria to find the cause.
Another possible cause of green nail syndrome is an abnormally lifted or separated fingernail. This is called onycholysis. This separation causes a subungual space where dirt can collect. This opens the door for Pseudomonas. Often, the condition affects people who work with their hands.
The infection is usually caused by a Pseudomonas bacterium in the nail bed. Symptoms include a thickened proximal fold, onycholysis of the distal nail plate, and a green nail bed. The bacterium has blue-green pigments that give the nails a green color.
The underlying fungus Pseudomonas – a common bacterium known to cause green nail syndrome – is responsible for the discoloration of the nail. Pseudomonas is usually the source of the infection, but it can also result from ungual trauma. The symptomatic condition generally affects one fingernail, although the adjacent nail may have an additional illness in some patients.
There is no cure for this condition, but the treatment depends on the underlying cause. Generally, you should avoid wearing artificial nail enhancements until the infection is treated. However, you should remove it from your nails and allow the nail to heal. Clear vinegar (not the balsamic variety) can be applied to the stained nail over several weeks or months.
Candida parapsilosis

A patient presenting with a green discoloration of the right thumbnail exhibited distal nail plate detachment. Microscopic examination revealed PAS-positive pseudohyphae and yeast. A culture of the nail plate for Candida species did not yield organisms; a fungal culture of the nail plate grew C. . Treatment included five cycles of oral itraconazole 200 mg twice daily. The patient showed no recurrence after three weeks of therapy.
One patient presenting with a discolored nail plate had been diagnosed with Candida, a form of bacterial-associated green nail syndrome. However, fungal etiologies have also been identified. In one case, a 70-year-old woman presented with an asymptomatic, diffuse green nail bed on her left fourth fingernail for five months. She had previously been prescribed tramadol for chronic back pain and losartan for an overactive bladder. The patient subsequently underwent treatment with topical mupirocin 2% ointment and a topical cream.
The clinical course of this disease is unpredictable and can occur in individuals with any underlying medical condition.
Generally, the infection begins at the proximal nail fold and may spread to the lateral margins of the nail. The periungual skin becomes erythematous and swollen, and a prominent gap between the nail plate and periungual tissue develops. The fungus can cause white, green, or black stripes on the nail plate and may lead to a persistent green nail syndrome.
The presence of Candida in the nail bed is usually the result of local underlying diseases, such as Raynaud’s syndrome or an occupational illness. However, the disease can be prevented by taking preventive measures. Keeping your hands warm can help you avoid acquiring an infection and prevent it in the future. Affected individuals can also consider taking antifungal medications to prevent it from spreading.
In one case, a 64-year-old woman developed a green nail plate in two months. The discoloration was localized to the proximal nail plate and gradually progressed to the distal margin. She had no previous nail disease or trauma, and the patient underwent topical acetic acid and ethyl lactate treatments without success.
Distal Candida infection may present with onycholysis and subungual hyperkeratosis. Distal Candida nail infection is difficult to differentiate from dermatophytosis. Despite its rarity, patients with DLSO often experience Raynaud’s phenomenon.
Why Would a New Toenail Grow Under a Healthy Toenail?

Your toenail grows out of a matrix, a small pocket under the skin that constantly forms new cells and lengthens the nail. The old and dead cells are forced to grow out of the matrix. The lunula, a crescent-shaped area on the bottom of your pin, is part of the matrix, and its presence does not indicate a healthy nail.
Ingrown toenails are caused by improper trimming.
Ingrown toenails are a painful condition. They can be caused by improper nail trimming, trauma, and lousy foot hygiene. These conditions also affect people who wear tight shoes or socks. Other potential causes include fungal infections and traumatic injuries. Luckily, this condition is easy to diagnose. Physical examination findings vary depending on the stage of the disease. Symptoms of ingrown toenails include pain, difficulty walking, and in some cases, complete inability to walk.
If left untreated, ingrown toenails can become infected. If you try to trim the nail’s corner, you can result in a fishhook deformity. Ingrown toenails can be painful and require surgical intervention. Treatment options include antibiotics, a cotton wick inserted under the infected toenail, and amputation. Surgical removal of the affected nail is necessary when the condition does not improve.
Fortunately, ingrown toenails are usually treatable at home. You can soak your feet in warm Epsom salt and apply an antibiotic cream., it’s best to avoid wearing tight toe box shoes. If you cannot avoid wearing shoes with a closed-toe box, you should soak your toes in the water for several minutes. Afterward, gently clip the affected area.
Ingrown toenails are painful and can cause severe pain and inflammation. They can be painful to remove, and the infection can lead to an infection. When infected, the toe becomes red and swollen and may turn darker than usual. You can also notice some bleeding or darkened skin near the affected area. Ingrown toenails are genetic and can run in families. As such, it’s essential to learn more about the condition and how to prevent it.
Toenail fungus causes debridement.

In addition to these, other types of fungi can cause nail infections, including Candida Albicans. In addition to these, individuals who suffer from poor foot hygiene and exposure to damp areas are at risk of developing this infection. People who suffer from athlete’s foot, diabetes, or walk barefoot may be particularly susceptible to this infection.
The early stage of the infection is crucial to the overall management of the condition. Proper foot hygiene can prevent fungal infections from forming in the first place, preventing them from worsening and preserving the appearance of your toenails. In addition to maintaining good foot hygiene, patients should visit a podiatrist for treatment if the condition has progressed to the stage where it requires surgical removal.
Treatment for fungal infections can be done by applying antifungal creams or lotions or wearing shoes that allow your toenails to breathe. Depending on the type of toenail fungus, oral medications and topical medications are the most common treatments. Treatment timelines will vary depending on the severity of the infection. However, most people can successfully treat their fungal infections without surgery.
If you suspect that you are suffering from a fungal infection, a doctor will examine your nails and take a sample of debris from under your nail for testing. This sample will be sent to a lab to identify the type of fungus responsible for the infection. Although toenail fungus can be challenging to remember, the fungus that infects your nail is often a component of another condition, such as psoriasis. A doctor will determine the exact nature of the infection and recommend the best treatment for the unique case.
Improper trimming

Sometimes an ingrown toenail will develop when you don’t correctly trim it. Ingrown toenails can grow under a healthy toenail due to trauma or infection. The new nail may grow under the old one and detach from the nail bed, leaving a space for a new toenail. If the pin has separated from the nail bed, it will continue to grow and eventually fall off. In this case, you should clip or remove the new toenail and consult a doctor if the situation persists.
Ingrown toenails are an uncomfortable problem. The nail digs into the skin, causing irritation and pain. If left untreated, it can cause an infection and lead to fungal infections and the loss of the nail, or even infection. While it can be treated at home, it is not recommended if you suspect an infection or have a high-risk foot condition.
If the condition persists, you should visit a doctor. The doctor can prescribe antibiotics or perform a surgical procedure to remove the affected nail. Home remedies may not be sufficient. A visit to the doctor is necessary if pain or discomfort persists or you’re having trouble performing activities such as walking or running. Surgical removal of the ingrown toenail may be required, but it will be an unnecessary expense.
Improper trimming can also cause an ingrown toenail. People who trim their toenails daily can often encourage the growth of an ingrown toenail by tapering the corners. Improper trimming can also lead to ingrown toenails as the toenail will curl down into the skin, causing the ingrown toenail to develop. Improper trimming also encourages the development of ingrown toenails if their shoes are too tight or too short.
Toenail fungus causes dermatophyte fungus.
There are several types of toenail fungi. These include candida onychomycosis, subungual onychomycosis, and white superficial onychomycosis. Typically, the fungi infect the skin and burrow under the nails. This type of infection is caused by a buildup of dermatophyte fungi.
There are several reasons that an individual is predisposed to developing onychomycosis. These factors include occlusive footwear, physical exercise, and communal showers. Additionally, onychomycosis may be caused by yeast. Although dermatophytes are the most common cause, they are not the only types of fungi that can infect your toenails.
The most common type is distal subungual onychomycosis, caused by dermatophyte fungi. This fungus begins in the nail bed and spreads from the edge to the center of the nail. If it applies to the pin, it will become crumbly. A doctor may recommend surgery, laser therapy, or topical treatments in severe cases.
While this type of infection is rare in children, it is common in adults. It is caused by dermatophyte fungi but can also be caused by yeast, mold, or other fungi. Older adults are particularly susceptible to toenail fungus because their nails become brittle and develop cracks. Furthermore, reduced feet’ circulation and immune system can make the infection even more difficult to detect.
Ingrown toenails pose a health risk.

Aside from being unsightly, ingrown toenails can also be a significant health hazard. They can be challenging to treat or remove altogether, whether caused by an ill-fitting pair of shoes or trauma to the toenail. Fortunately, there are several ways to prevent ingrown toenails and alleviate symptoms. Read on for some tips.
A common cause of ingrown toenails is wearing shoes with tiny toes or too tight socks. In rare cases, these infections can even lead to gangrene, a condition whereby tissue dies from lack of blood supply. Fortunately, this is a rare complication, but it is still a serious concern. A lack of air exposure can also make the wound harder to heal.
The main symptoms of an ingrown toenail include pain, swelling, and redness. In extreme cases, ingrown toenails may cause a toe to become painful and inflamed. The condition can also lead to an infection, so it is essential to seek medical attention as soon as you notice a problem. Treatment options for ingrown toenails depend on the severity of the condition. A physician can prescribe an antibacterial cream to help treat the infection.
The treatment of ingrown toenails can range from home remedies to surgical treatments. While home remedies are safe and effective, medical care is recommended for more severe cases or if there is a high risk of infection. Those with high-risk medical conditions such as diabetes, nerve damage in the foot, and poor circulation may need to see a podiatrist for proper diagnosis and treatment.