- How Bad Should Your Skin Be Before You See a Dermatologist?
- Symptoms of psoriasis
- Symptoms of melanoma
- Should I Go to a Plastic Surgeon Or a Dermatologist For Skin Cancer Treatment?
- Cosmetic dermatologists provide non-invasive solutions.
- Plastic surgeons excise complex lesions.
- GPs excise small, low-risk skin cancers
- Choosing between a plastic surgeon and a dermatologist for skin cancer
How Bad Should Your Skin Be Before You See a Dermatologist?

If you’re worried that you may have a skin condition, you may want to see a dermatologist. Brown spots are a serious concern and can result in serious health risks. The following are symptoms to look for when deciding whether you should see a dermatologist. In some cases, the brown spots can be dangerous or even cancerous. If you’re worried about melanoma, you should also seek medical attention as soon as possible.
Symptoms of psoriasis

You should know several things about psoriasis before you visit a dermatologist. The most common form of the disease is chronic plaque psoriasis, although there are many subtypes of psoriasis. Although psoriasis is not contagious, genetics play an essential role. There are many causes of psoriasis, and research continues to find the exact cause.
Among the symptoms of psoriasis, one of the most common is joint pain. Joint pain is common for people with psoriasis, but if you experience any joint swelling. Inflammatory reactions accelerate the production of skin cells and produce thick, scaly plaques. Luckily, there is no need to worry – most dermatologists have seen many patients suffering from psoriasis.
When you see a dermatologist for psoriasis, they will want to know about your symptoms and how you have managed them. They can provide you with reassurance and answers based on the latest research. If you are not comfortable with your current dermatologist, consider switching to a specialist with expertise in psoriasis.
Among the symptoms of psoriasis are red, itchy patches on the skin. They are covered in silvery-white scales and are usually accompanied by itchiness. In addition to skin, psoriasis can also affect nails, joints, and the face. Skin folds and creases may become involved, and the patches can turn thicker over time. A dermatologist will recommend that you treat the condition if it is not severe.
While your dermatologist will conduct a skin exam, they may use a biopsy and ask you questions about your lifestyle and family history to make a more accurate diagnosis. Before you visit the dermatologist, write down your symptoms and make a list of questions for the doctor. They will want to see the condition, but it is essential to remember that the most effective psoriasis treatment is one that works for you.
Some types of psoriasis require the use of topical medications. With light therapy, these include corticosteroids, vitamin D, and salicylic acid, which reduce inflammation and itching in the skin. The effectiveness of topical treatments depends on the severity of the disease. You may need more than one visit to a dermatologist.
Because psoriasis affects the skin, it should be evaluated by a dermatologist as soon as possible. If it does not improve on its own, your condition may signify more severe complications. Psoriasis can lead to other health problems, such as psoriatic arthritis, which affects joints and limits movement. Watching your weight would help since psoriasis can cause rapid weight fluctuations and obesity.
Your dermatologist may prescribe oral medications to treat psoriasis. However, you should consult a dermatologist before using new drugs, as new treatments may interfere with your treatment plan. In addition, natural approaches may worsen symptoms. Always consult a dermatologist before making changes to your current treatment plan. The NPF Patient Navigation Center can help you find a dermatologist in your area.
Symptoms of melanoma

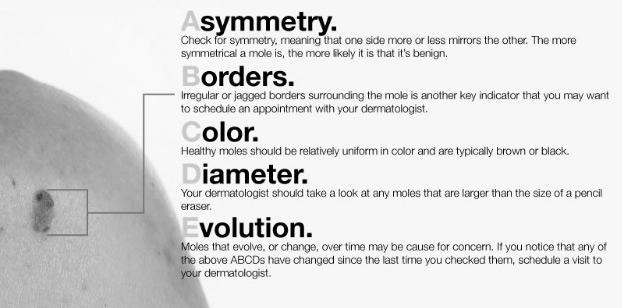
If you’ve noticed new growth or changes in your skin, you should see your dermatologist. These are all potential signs of melanoma. A change in old-growth or sore may be another warning sign. To get a better idea of your chances of having melanoma, consider the A-B-C-D-Es of melanoma.
Although melanomas are usually black or dark brown, there are other signs to look for before seeing a dermatologist. For example, a new mole appearing on your skin could signify more advanced melanoma. Moreover, bleeding from the mole may indicate more advanced melanoma. In this case, your dermatologist will ask you about other symptoms of melanoma so that they can better diagnose your condition.
Another symptom of melanoma is the presence of a suspicious mole that hasn’t gone away. It is essential to report sores that won’t go away or other unusual bumps on your skin. If the sore is growing too quickly, you should see a dermatologist as soon as possible. Your dermatologist can perform melanoma surgery in his office or refer you to a dermatologist for a second opinion.
Imaging tests may be necessary for advanced cases of melanoma. This type of test involves taking samples of cancer cells through fine needle aspiration. Your dermatologist will use the results of these tests to devise a treatment plan that is right for your condition. For severe cancer, you may need the services of a team of specialists, including a dermatologist and an oncologist.
There are many signs of melanoma. Although it typically occurs in the exposed areas of the body, it can also form in unexposed areas. In addition to the skin, melanoma can also occur in the eyes, mouth, the lining of the nose, digestive tract, urinary tract, and genital area. If you notice any of these signs, it’s essential to see your dermatologist as soon as possible.
It is essential to understand that melanoma can spread rapidly and become life-threatening within six weeks. While it is deadly once it has spread to other parts of the body, it can still be treatable if caught early. By learning the symptoms of melanoma before you see a dermatologist, you can protect yourself from the deadly consequences. You can learn how to spot these symptoms and avoid the costly mistake of a skin cancer diagnosis.
Some warning signs of melanoma can be easy to detect:
- Look for irregular or asymmetrical moles.
- Look for changes in the edges. They may be lumpy or uneven.
- If the skin lesion bleeds or oozes, it could be melanoma.
Fortunately, most melanomas do not cause pain.
Depending on your situation, your dermatologist may decide to biopsy a mole that you think is suspicious. It makes it easier for the doctor to monitor its changes over time. The dermatologist may perform a skin biopsy in the same appointment or another one. You may also need to see your dermatologist again in three months for a follow-up. If you notice any changes in the mole’s size, show it to your doctor.
Another way to check for a mole is with a hand mirror. If you don’t have a hand mirror, you may want to ask someone to help you study for moles. Even if they’re small, melanomas can occur in nearly any part of the body. Taking care of these changes is crucial to your health and survival. If you don’t notice any of these signs or symptoms, it may be a sign of melanoma.
Before seeing a dermatologist, you should do a self-examination regularly to check for melanomas on your skin. This way, you’ll have a better chance of catching it before seeing a dermatologist. If you’re already diagnosed with melanoma, the dermatologist will be able to identify your skin cancer if it has spread to lymph nodes.
If you’ve discovered melanoma on your skin, your dermatologist can perform surgery to remove it. A dermatologist can perform a melanoma surgery in the office while you’re still awake. The dermatologist will then numb the affected area and cut the surrounding normal skin. Various types of excision are available. You may undergo surgery to remove cancer or opt for palliative care.
Should I Go to a Plastic Surgeon Or a Dermatologist For Skin Cancer Treatment?
When it comes to skin cancer, which is better for the treatment? Both plastic surgeons and dermatologists are well-qualified to perform the procedure. Dermatologists focus on less-invasive solutions, while plastic surgeons typically perform surgical procedures. Regardless of the type of treatment, a plastic surgeon will likely be more experienced and skilled in complex lesions. If you’re wondering how to choose between a dermatologist and a plastic surgeon, you’ll want to take the time to do your research.
Cosmetic dermatologists provide non-invasive solutions.

When you want to improve the appearance of your skin, you may have several options. Cosmetic dermatologists offer advanced solutions and safe and non-invasive procedures to address your concerns. These options may include laser hair removal, fillers, and chemical peels. Considering cosmetic dermatology, you should know what is involved before undergoing the procedure. Cosmetic dermatologists are also experts in the latest technology and techniques to give you the best results with the least amount of downtime.
A cosmetic dermatologist first evaluates the health of the skin. If your skin is prone to pigmentation problems, resurfacing may be the answer. If fine lines and wrinkles have affected your appearance, a dermatologist may suggest neurotoxins or space-occupying fillers improve your appearance. If your concerns are age-related, you may wish to discuss other procedures, such as lip augmentation, which helps make lips look fuller and younger.
A cosmetic dermatologist will develop a customized treatment plan with you and your aesthetic dermatologist. Rapid results will increase patient confidence and encourage continued treatments. Because the treatments are non-surgical, you won’t have to endure painful recovery time. Even if your desired results are instant, your team will need to educate you about the available options. They will be able to answer all of your questions about your specific situation and the treatments available.
And because many patients have heard about “miracle treatments,” you should make sure your dermatologist is aware of the risks and limitations associated with the procedures before you undergo any treatment. So, make sure you choose a dermatologist with a good reputation.
Plastic surgeons excise complex lesions.

This study aimed to determine whether the removal of NMSC. The study excluded MMS patients before plastic surgery and those who underwent only punch biopsies or reconstruction. The study also excluded patients who had only one type of NMSC – congenital nevi – and those who had experienced two or more plastic surgeries. It found that SE was superior to conventional shave biopsies for removing this type of lesion.
Skin cancer is one of the most common forms of cancer in the U.S. and can be dangerous and disfiguring. While some types of skin cancer are easily excised, others require extensive surgery and disfigurement. Plastic surgeons excise most facial lesions. Mohs surgery, in contrast, is disfiguring and almost always requires reconstructive surgery to restore the patient’s appearance. Nevertheless, it is essential to understand that plastic surgeons are not limited to treating skin cancer and can perform many surgical procedures.
While GPs can safely excise many types of skin lesions, plastic surgeons may be the most appropriate choice for complex lesions. Although they may not be required to perform all kinds of excisions, dermatologists are often the most experienced and skilled at handling complex lesions. In addition to their excellent diagnostic skills, dermatologists are the most likely to be involved in the excision of a complex lesion; success rates are the best.
Excisions can be done in the office without or under general anesthesia at a hospital. The goal of excision is to remove the entire growth, whether it’s an organ or part of the body. It can be an effective method for diagnosing and treating many medical conditions. In addition, surgical excisions can be performed on an outpatient basis.
GPs excise small, low-risk skin cancers

It is unclear if GPs are increasingly excising small, low-risk skin cancers. Researchers have conducted studies of high-risk BCC excisions in primary care settings. A 2010 study of three-month data from Lothian plastic surgeons and dermatologists found that 63% of GP-excised BCCs had features indicative of high-risk disease.
GPs can diagnose most NMSCs on clinical grounds, but excision remains the gold standard for skin cancers. For uncomplicated skin lesions, the gold-standard excision method is an elliptical incision with a three to four-mm margin. Other treatments include liquid nitrogen, imiquimod, and photodynamic therapy. GPs should refer patients with complicated or dangerous skin cancers to specialists. GPs should not prescribe prophylactic antibiotics for uncomplicated NMSCs, especially in young patients, immunocompromised patients, and those with a history of skin conditions.
GPs are more likely to perform minor surgery on NMSC than specialists in Australia. The number of minor surgeries performed by GPs has grown significantly in recent years. Further research is needed to assess the quality of GP care in skin cancer management. As the incidence of NMSC continues to rise, GPs will need to play an increasingly significant role in the direction of these cancers.
There are several complications with the diagnosis and excision of BCCs. GPs must be able to correctly identify a high-risk BCC and perform it safely and effectively. Despite these challenges, the NICE 2010 guidance outlines how to improve GP practice in skin cancer management. Further, this guidance is not intended to replace dermatology.
GPs are the most common providers of skin cancer care. While this is true, referral pathways to dermatology services are often unclear. Can delay timely access to secondary care. Improved communication between GPs and dermatologists would ensure that outpatient management of skin neoplasms is appropriate. If you or a family member has a suspicious skin lesion, visit a dermatologist for a proper diagnosis and treatment.
Choosing between a plastic surgeon and a dermatologist for skin cancer

When it comes to treating skin cancer, there are overlaps between dermatology and plastic surgery. While dermatologists can treat most cases in their offices, special situations require coordination with a plastic surgeon. This article provides tips for dermatologists referring patients to plastic surgeons. Below are some of the most important differences between the two physician groups. Before choosing a doctor, take the time to understand how skin cancer is diagnosed.
First, a dermatologist has better surgical skills than a plastic surgeon. Dermatologists are highly trained to identify skin cancer in its early stages. They also tend to use narrower margins to preserve aesthetics and protect vital neurovascular structures. However, the difference in these procedures is not so significant that a patient should choose a surgeon based on their specialty.
When it comes to treating skin cancer, a dermatologist performs Mohs surgery. Unlike a plastic surgeon, a dermatologist does not use radiation. He performs surgery to remove skin cancer. The doctor will also examine any normal-looking skin that the tumor may cover. If cancer cells are found in the surrounding healthy skin, a dermatologist may perform a more extensive procedure, such as Mohs surgery.
While both physicians can excise skin lesions, a dermatologist’s diagnosis is more accurate. He is also more likely to perform the excision in complex cases and difficult to treat areas. Moreover, a dermatologist has the highest disease-free survival and overall survival rate. Plastic surgeons have better surgical skills and tend to be more experienced.
Choosing between a plastic surgeon and specialized skin cancer treatment depends on your particular condition and medical history. A dermatologist can treat superficial skin cancers in an office setting, but more complex cases may require the expertise of several health care providers. The specialists on the healthcare team can answer important questions and provide valuable information about your diagnosis. In addition, you should consider the type of cancer and the level of involvement of nerves.